Coitus and conception are the initial stages that occur in humans that allow for the establishment of pregnancy. Sexual intercourse that results in the deposition of sperm in the vagina at the level of the cervix is known as coitus.
For coitus to occur humans need to be sexually aroused. Sexual arousal is then followed by a series of phases. These phases are:
- Excitement phase
- Plateau phase
- Orgasmic phase
- Resolution phase.
In this article, we shall look at the various phases of coitus and some clinical conditions.
Male Sexual Response
The changes that occur to allow coitus involve genital and systemic alterations in both sexes. The first part of sexual stimulation in a male results in the production of an erection.
An erection may be produced due to psychogenic or somatogenic stimuli. Psychogenic stimuli cause stimulation of efferent nerves to the penis via the limbic system from sensory cues such as images. Somatogenic stimuli cause this same stimulation but through sensations such as touching the penis.
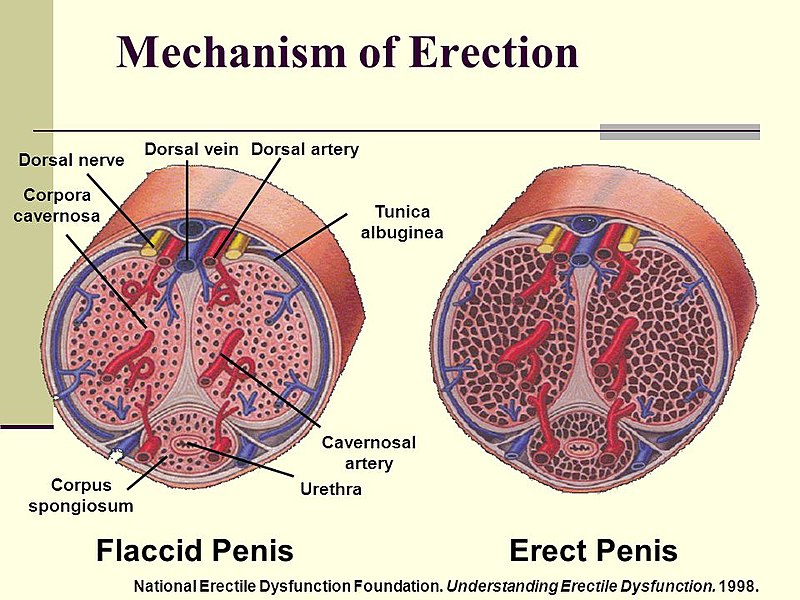
Fig 1 – Diagram to show the engorgement of blood vessels involved in producing and maintaining an erection in males
The plateau phase in males results in an increase in penile erection, an increase in the size of the testicles and a rise in heart rate and blood pressure.
Following on from the plateau phase there is the orgasmic phase. The orgasmic phase has two parts: emission and ejaculation. Emission is where several structures contract to mix the contents of ejaculate. Ejaculation is where semen is then expelled from the prostatic urethra due to muscular contractions.
The final part of the sexual response cycle is the resolution phase and in males, this is split into two stages. The first stage results in the penis reducing from full erection to 50% larger than its unstimulated size and the second, longer phase, results in the penis reducing to its normal unstimulated size.
Stages of Male Sexual Function:
| Males | Nervous system stimulated | Consequence | |
| Coitus | |||
| Excitement phase | Sacral parasympathetic neurons | Arteriolar vasodilation in corpora cavernosa which increases penile blood flow
Penile filling (latency) Penile tumescence (erection) |
|
| Plateau phase | Sacrospinous reflex | Contraction of ischiocavernosus
Venous engorgement and decreased arterial inflow Testes become completely engorged and elevated Stimulates secretion from accessory glands which will make up 5% of ejaculate Lubricates distal urethra and neutralises acidic urine in the urethra |
|
| Orgasmic phase | Emission | Thoracolumbar sympathetic reflex | Contraction of smooth muscles in ductus deferens, ampulla, seminal vesicle and prostate
Internal and external urethral sphincters contract Semen pooled in the urethral bulb |
| Ejaculation | Spinal reflex with cortical control (L1, L2 sympathetic) | Contraction of glands and ducts
Contraction of urethral sphincter Filling of the internal urethra stimulates the pudendal nerve, which contracts genital organs, ischiocavernosus and bulbocavernosus – resulting in the expulsion of semen |
|
| Resolution phase | Thoracolumbar sympathetic pathway | Contraction of arteriolar smooth muscle in corpora cavernosa
Increased venous return leads to detumescence flaccidity which results in the refractory period |
|
Table 1 – Summary of the male phases of coitus
Female Sexual Response
The autonomic nervous system that controls the four parts of coitus is the same in males and females, however, the responses of the genital organs are different.
Within females, the excitement phase results in anatomical changes that increase the circumference of the vaginal diameter at the level of the pelvis and lubricate the vagina for penile entry.
Following the excitement phase, the plateau phase results in the labia minora becoming red in appearance as well as the respiratory rate, heart rate and blood pressure increasing.
Within females, the orgasmic phase does not include emission and ejaculation. The orgasm includes contraction of the lower third of the vagina and can extend to the whole vagina and uterus. The final phase of resolution encompasses several changes that result in the return of the structures to normal unstimulated states.
Stages of Female Sexual Function:
| Females | Nervous system stimulated | Consequence |
| Coitus | ||
| Excitement phase | Sacral parasympathetic neurons | Vasocongestion
Vaginal lubrication Clitoris engorges with blood Uterus elevates Increase in muscle tone, heart rate and BP Inner two-thirds of the vagina lengthens and expands |
| Plateau phase | Sacrospinous reflex | Further increase in muscle tone, heart rate and BP
Labia minora deepens in colour Clitoris withdraws under hood Bartholin gland secretion to lubricate vestibule for entry of penis Uterus is fully elevated and organismic platform forms in the lower one-third of the vagina |
| Orgasmic | Spinal reflex with cortical control (L1, L2 sympathetic) | The orgasmic platform contracts rhythmically 3-15 times
Uterus contracts, anal sphincter contracts |
| Resolution phase | Thoracolumbar sympathetic pathway | Clitoris descends and engorgement subsides
Labia return to unaroused colour and size Uterus descends to unaroused position Vagina shortens and narrows back to the unaroused state No refractory period so multiple orgasms are possible |
Table 2 – Summary of the female phases of coitus
Male Vs Female Sexual Response
There are several differences in the physiological sexual response of males and females:
- Emission and ejaculation do not occur in the female
- Females are capable of several orgasms and the orgasm may last relatively longer than that of a male
- Females can reach the plateau phase and sustain it then return to an unstimulated state without orgasm
Clinical Relevance – Ageing and the Sexual Response
Several changes occur in females as a result of ageing:
- Reduced vasocongestion response, causing reduced vaginal lubrication
- Vaginal and urethral tissue lose elasticity
- Length and width of the vagina decrease which reduces the expansile ability of the inner vagina during arousal
- The number of orgasmic contractions is often reduced
- More rapid resolution
Clinical Relevance – Sexual Dysfunction
Sexual dysfunction can be caused by a change in desire or arousal. The most common type of sexual dysfunction is when there is a problem with desire. Below are several types of sexual dysfunctions caused by an abnormality in desire:
- Hypoactive – little or no interest in sex
- Aversion – revulsion or fear of sex
- Hyperactive
- Nymphomaniac
- Kluver Bucci syndrome
Impotence
In males, a problem with arousal is called impotence. Impotence can be caused by descending inhibition of spinal reflexes due to psychological problems, tears in the fibrous tissue of corpora cavernosa, vascular abnormalities (atherosclerosis and diabetes) and certain drugs. Viagra (sildenafil) can be prescribed for males and works by inhibiting cGMP breakdown and results in an increased nitric oxide action that produces an erection.
Sperm abnormalities may be another reason for sexual dysfunction and this could be a low level of sperm within the ejaculate (oligospermia) or sperm morphological defects.
Vaginismus
Vaginismus is a condition that may affect individuals with vaginas. It is described as “involuntary contraction of the vaginal musculature, which usually leads to a failure in penetration”. This can be as a result of a number of psychosocial factors in an individual’s life including stress, previous abuse, or substance misuse.
