The lie, presentation and position of a fetus are important during labour and delivery.
In this article, we will look at the risk factors, examination and management of abnormal fetal lie, malpresentation and malposition.
Definitions
- Lie – the relationship between the long axis of the fetus and the mother.
- Longitudinal, transverse or oblique
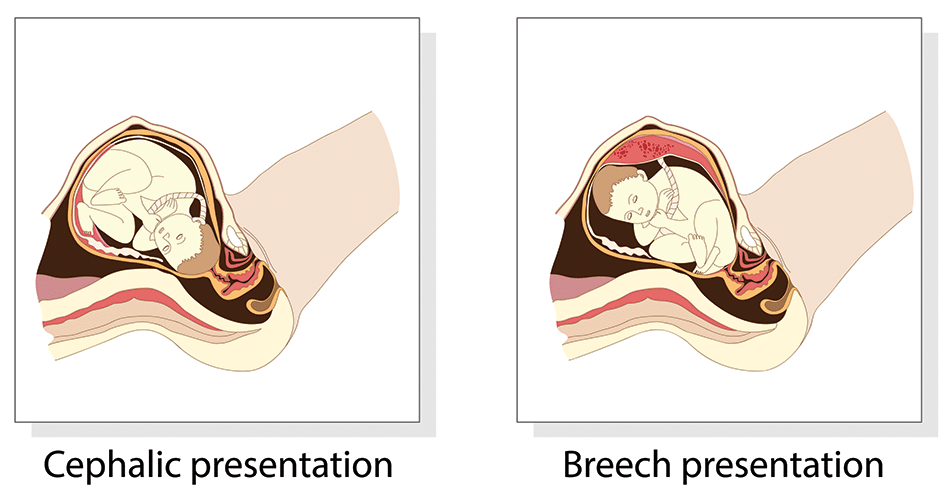
- Presentation – the fetal part that first enters the maternal pelvis.
- Cephalic vertex presentation is the most common and is considered the safest
- Other presentations include breech, shoulder, face and brow
- Position – the position of the fetal head as it exits the birth canal.
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) – this is ideal for birth
- Other positions include occipito-posterior and occipito-transverse.
Note: Breech presentation is the most common malpresentation, and is covered in detail here.
Risk Factors
The risk factors for abnormal fetal lie, malpresentation and malposition include:
- Prematurity
- Multiple pregnancy
- Uterine abnormalities (e.g fibroids, partial septate uterus)
- Fetal abnormalities
- Placenta praevia
- Primiparity
Identifying Fetal Lie, Presentation and Position
The fetal lie and presentation can usually be identified via abdominal examination. The fetal position is ascertained by vaginal examination.
For more information on the obstetric examination, see here.
Lie
- Face the patient’s head
- Place your hands on either side of the uterus and gently apply pressure; one side will feel fuller and firmer – this is the back, and fetal limbs may feel ‘knobbly’ on the opposite side
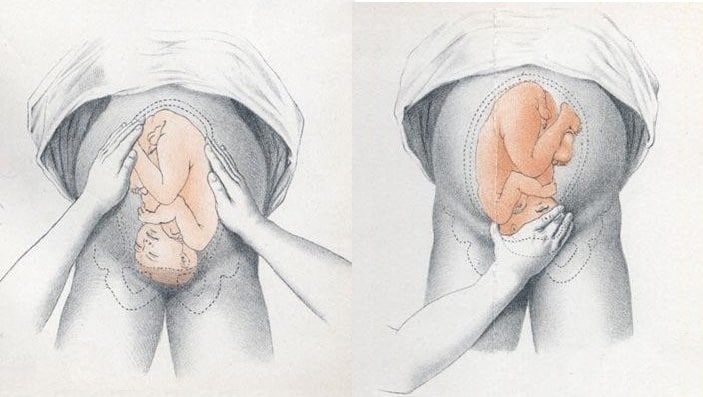
Presentation
- Face the patient’s head
- Palpate the lower uterus (above the symphysis pubis) with the fingers of both hands; the head feels hard and round (cephalic) and the bottom feels soft and triangular (breech)
- You may be able to gently push the fetal head from side to side
The fetal lie and presentation may not be possible to identify if the mother has a high BMI, if she has not emptied her bladder, if the fetus is small or if there is polyhydramnios.
Position
During labour, vaginal examination is used to assess the position of the fetal head (in a cephalic vertex presentation). The landmarks of the fetal head, including the anterior and posterior fontanelles, indicate the position.
Investigations
Any suspected abnormal fetal lie or malpresentation should be confirmed by an ultrasound scan. This could also demonstrate predisposing uterine or fetal abnormalities.
Management
Abnormal Fetal Lie
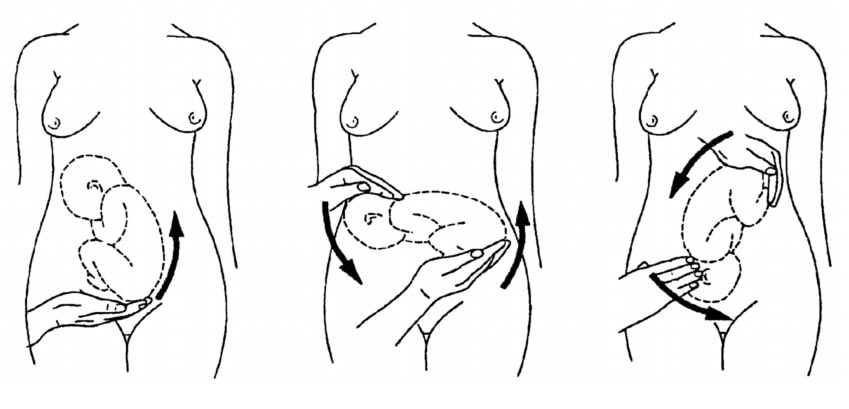
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted – ideally between 36 and 38 weeks gestation.
ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen.
It has an approximate success rate of 50% in primiparous women and 60% in multiparous women. Only 8% of breech presentations will spontaneously revert to cephalic in primiparous women over 36 weeks gestation.
Complications of ECV are rare but include fetal distress, premature rupture of membranes, antepartum haemorrhage (APH) and placental abruption. The risk of an emergency caesarean section (C-section) within 24 hours is around 1 in 200.
ECV is contraindicated in women with a recent APH, ruptured membranes, uterine abnormalities or a previous C-section.
Malpresentation
The management of malpresentation is dependent on the presentation.
- Breech – attempt ECV before labour, vaginal breech delivery or C-section
- Brow – a C-section is necessary
- Face
- If the chin is anterior (mento-anterior) a normal labour is possible; however, it is likely to be prolonged and there is an increased risk of a C-section being required
- If the chin is posterior (mento-posterior) then a C-section is necessary
- Shoulder – a C-section is necessary
Malposition
90% of malpositions spontaneously rotate to occipito-anterior as labour progresses. If the fetal head does not rotate, rotation and operative vaginal delivery can be attempted. Alternatively a C-section can be performed.