Varicella zoster is a DNA virus responsible for:
- Chickenpox (also known as varicella) – a result of primary infection.
- Shingles (also known as herpes zoster) – a result of viral reactivation.
Most of the antenatal population (~90%) is seropositive for the varicella zoster IgG antibody (due to previous exposure). These women therefore have immunity to repeat primary infection. As a result, chickenpox is relatively uncommon during pregnancy – with an incidence of about 3 in 1000.
Despite this low incidence, the infection remains a serious consideration in pregnancy. Whilst the virus causes a mild illness in children, if contracted during pregnancy there is increased morbidity and mortality for both mother and fetus.
In this article, we shall look at the clinical features, investigations and management of varicella zoster infection during pregnancy.
Clinical Features
Primary varicella zoster infection typically presents with fever, malaise and a pruritic maculopapular rash. The rash characteristically becomes vesicular and crusts before healing.
The incubation period for the virus is 10-21 days. The woman is infectious from 48 hours prior to the rash to until the vesicles have crusted.
Infection is associated with pneumonia, hepatitis, and encephalitis – accounting for the 2% mortality in mothers.
Investigations
Primary varicella zoster infection is typically a clinical diagnosis, made on the basis of history and examination. In cases where the diagnosis is in doubt, there are two main investigations that can be used:
- Immunofluorescence of basal epithelial cells scrapped from vesicle.
- PCR for varicella zoster DNA.
To determine immunity status, women can be tested for IgM and IgG antibodies to varicella zoster. If present, they indicate the woman has immunity against the virus (usually from previous infection or vaccination).
Management
When discussing management, there are two common scenarios to consider; (i) management of a woman who has encountered someone infectious with varicella zoster, and (ii) management of a woman with confirmed varicella zoster.
Maternal Suspected Varicella Contact
In a case where a pregnant woman has encountered a person infectious with varicella zoster, previous exposure should be asked about:
- If mother describes previous primary varicella zoster infection – assume immunity. No further action is required.
- If no previous infection – varicella zoster IgG testing is required to confirm immunity status.
If not immune and less than 20 weeks gestation, the woman should receive varicella zoster immunoglobulin (VZIG) within 10 days of the contact, and before the onset of rash.
If not immune and more than 20 weeks gestation, the woman can receive either VZIG, or alternatively Aciclovir can be given from days 7 to 14 following exposure.
These women should then be managed as potentially infectious from 8 to 28 days.
Maternal Chickenpox
Aciclovir (800mg PO 5tds) should be prescribed in patients presenting within 24 hours of rash onset and at >20 weeks gestation. Consider aciclovir prescription in mothers <20 weeks.
The mother should be counselled about the symptoms of pneumonia, neurological signs and haematological rash – and instructed to attend hospital immediately should they occur.
In addition, she should be referred to a fetal medicine specialist, with serial ultrasound examinations beginning at 5 weeks post infection to identify any fetal abnormalities.
Varicella Vaccination
If a woman is found to be seronegative for varicella zoster IgG, pre-pregnancy or postpartum vaccination should be considered. Vaccination is not recommended during pregnancy as a matter of caution.
Complications
Varicella of the Newborn
If maternal chickenpox occurs within the last 4 weeks of the pregnancy, there is significant risk (50%) of varicella infection of the newborn. This can be asymptomatic.
The route of infection can be:
- Transplacental
- Vaginal
- Direct contact after birth
Varicella of the newborn is treated with varicella-zoster immunoglobulin (VZIG) ± aciclovir.
Fetal Varicella Syndrome
Fetal varicella syndrome is caused by subsequent reactivation of the virus in utero as herpes zoster. This reactivation only occurs when the fetus is infected by maternal varicella before 20 weeks gestation.
Only 1-2% of pregnancies infected before 20 weeks gestation will develop fetal varicella syndrome. It is characterised by:
- Skin scarring in a dermatomal distribution
- Eye defects
- Microphthalmia
- Choriorenitis
- Cataracts
- Optic atrophy
- Hypoplasia of the limbs
- Neurological Abnormalities
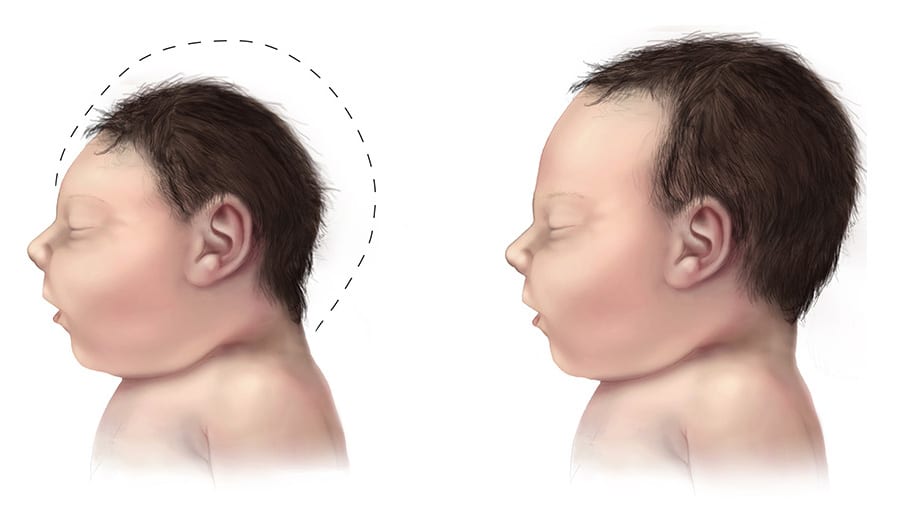
- Microcephaly
- Cortical and spinal cord atrophy
- Seizures
- Horner’s Syndrome