Gestational trophoblastic disease (GTD) is a term used to describe a group of pregnancy-related tumours. They can be divided into two main groups:
- Pre-malignant conditions (more common) – such as partial molar pregnancy and complete molar pregnancy.
- Malignant conditions (rarer) – such as invasive mole, choriocarcinoma, placental trophoblastic site tumour and epithelioid trophoblastic tumour.
In this article we will discuss the risk factors, clinical features and management of gestational trophoblastic disease.
Pathophysiology
Molar Pregnancies
In normal conception, the fetus is formed from 23 maternal chromosomes and 23 paternal chromosomes. A molar pregnancy arises from an abnormality in chromosomal number during fertilisation:
- Partial molar pregnancy – where one ovum with 23 chromosomes is fertilised by two sperm, each with 23 chromosomes. This produces cells with 69 chromosomes (triploidy).
- Note: A partial mole may exist with a viable fetus. The fetus and placenta are usually triploid, however mosaicism can exist where the fetus has a normal karyotype and the triploidy is confined to the placenta.
- Complete molar pregnancy – where one ovum without any chromosomes is fertilised by one sperm which duplicates, or (less commonly) two different sperm. This leads to 46 chromosomes of paternal origin alone.
These tumours are usually benign, but can become malignant – invading into the uterine myometrium, and disseminating around the body. These are known as invasive moles.
Other Types of Gestational Trophoblastic Disease
There are three main other forms of gestational trophoblastic disease:
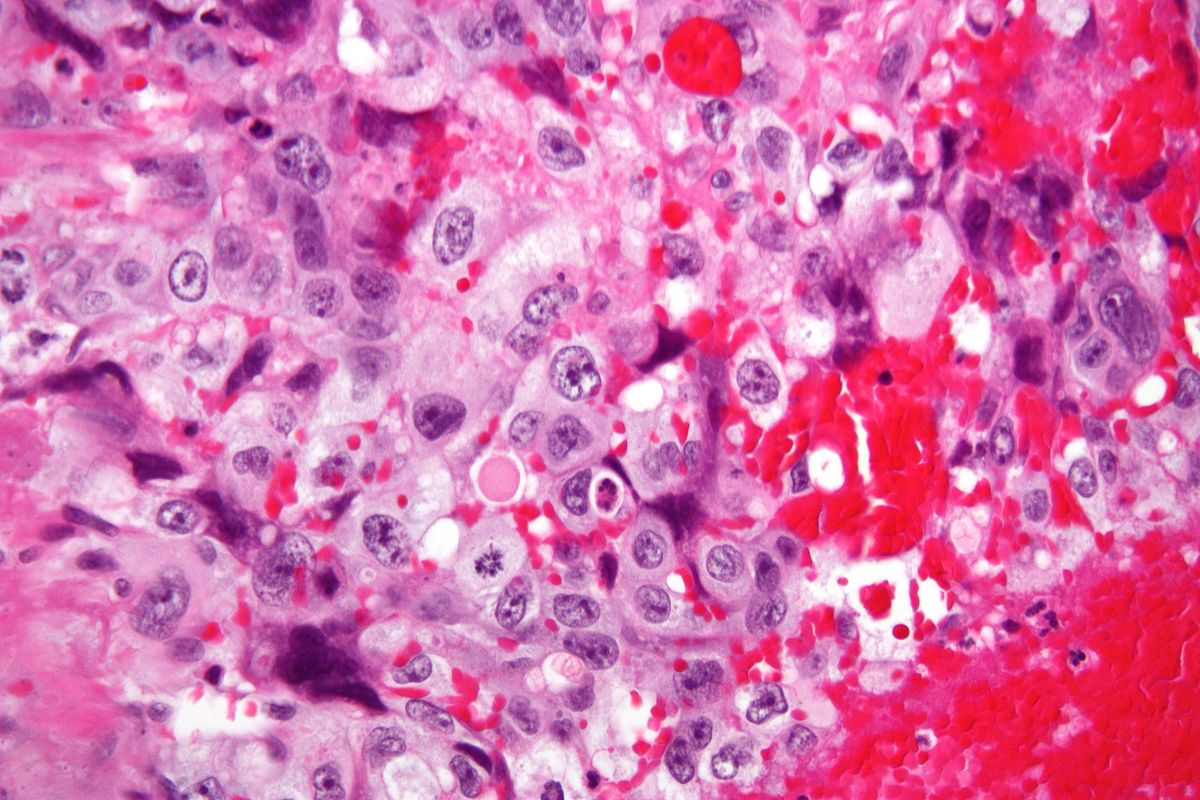
- Choriocarcinoma – a malignancy of the trophoblastic cells of the placenta. It commonly, but not exclusively, co-exists with a molar pregnancy.
- This type of GTT characteristically metastasises to the lungs.
- Placental site trophoblastic tumour – a malignancy of the intermediate trophoblasts, which are normally responsible for anchoring the placenta to the uterus.
- They can occur after a normal pregnancy (most common), a molar pregnancy or a miscarriage.
- Epithelioid trophoblastic tumour – a malignancy of the trophoblastic placental cells, which can be very difficult to distinguish from choriocarcinoma. It mimics the cytological features of squamous cell carcinoma.
Risk Factors
The major risk factors for gestational trophoblastic disease are:
- Maternal age <20 or >35
- Previous gestational trophoblastic disease (this risk is not decreased by a change of partner)
- Previous miscarriage
- Use of the oral contraceptive pill
Clinical Features
Molar pregnancies commonly present with vaginal bleeding and abdominal pain early in pregnancy. On examination, the uterus can be larger than expected for gestation, and of a soft, boggy consistency. Occasionally, molar vesicles can shed per vagina.
The diagnosis is usually made by ultrasound. However, if undiagnosed, later symptoms include:
- Hyperemesis – because there is an increased titre of B-hCG which is thought to be linked to nausea in pregnancy.
- Hyperthyroidism – gestational thyrotoxicosis due to stimulation of the thyroid by high HCG levels.
- Anaemia
Later in pregnancy, a ‘large for dates’ uterus may be noted on examination.
Investigations
The most common investigations in the assessment of suspected GTD involve B-hCG measurements, ultrasound, and histological examination:
- Urine B-hCG – typically measured in cases of persistent post-partum bleeding.
- Note: any urinary pregnancy test will remain positive for a number of weeks following delivery as B-hCG is cleared gradually.
- Blood B-hCG levels – markedly elevated at diagnosis, and also used in the monitoring of gestational trophoblastic disease.
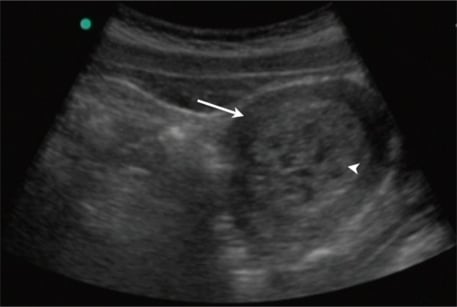
- Ultrasound Scan – a complete mole has a granular or snowstorm appearance with a central heterogeneous mass and surrounding multiple cystic areas/vesicles.
- However, this is not diagnostic of other forms of GTD – as partial moles may not have this distinctive ultrasound appearance.
- Histological examination of the products of conception – this is performed post-treatment on molar pregnancies, and all non-viable pregnancies to confirm diagnosis and plan follow up.
- Where a partial mole is suspected and the fetus is viable, if patients opt to continue the pregnancy, placental histology should be performed after delivery.
In cases where metastatic spread is suspected, staging investigations are required. This may include MRI, CT chest-abdomen-pelvis and/or pelvic ultrasound.
Management
In the UK, women diagnosed with gestational trophoblastic disease should be registered with a GTD centre for follow-up and monitoring in future pregnancies.
The specific management is dependent on the exact type of tumour.
Molar Pregnancy
The Royal College of Obstetricians and Gynaecologists recommend suction curettage as the most effective treatment for complete moles and non-viable partial moles. There is a theoretical risk of embolisation of the trophoblastic tissue if medical management with oxytocic agents is used.
However, if the partial mole is of a greater gestation with fetal development, and is not conducive to surgical evacuation, medical evacuation should be recommended – with a urinary B-hCG measurement performed 3 weeks post-treatment.
In all cases, anti-D prophylaxis is recommended post-evacuation if the mother is Rhesus negative. Chemotherapy may be required after evacuation if the B-hCG level does not fall (see below).
Other types of GTD
In cases of malignant gestational trophoblastic disease, or partial/complete mole that has not resolved, the woman should be referred to a specialist GTD treatment centre.
Single or multiple agent chemotherapy +/- surgery is the mainstay of treatment.