Sexual health can be a delicate subject for some patients therefore it is important to treat any information divulged with sensitivity and respect. Clinicians need to be comfortable asking the clinically relevant questions that make up the sexual history.
Do not make assumptions e.g. a patient’s sexual orientation, and be sure to clarify language used e.g. ‘sex’ may have different meanings for different people.
In this article we shall be looking at the components that make up a basic sexual history, many of which overlap with the gynaecological history.
History of Presenting Complaint
Use open questioning to allow the patient to fully elaborate on their problem. Ask about impact on daily life and how it is currently being managed.
Information to elicit from the presenting complaint includes:
- Type and site of symptoms
- Timing
- Onset and duration
- Cyclical – are symptoms associated with menstruation?
- Intermittent or continuous
- Exacerbating or relieving factors
- Previous episodes – including any investigations and treatments
- Other associated features
Symptoms
After exploring the history of the presenting complaint, inquire about the common symptoms of sexually transmitted diseases.
Vaginal Bleeding
Abnormal vaginal bleeding exists in three main forms:
- Intermenstrual (between menstrual periods) – this may indicate infection or non-sexually transmitted causes including malignancy, fibroids, endometriosis, hormonal contraception
- Post-coital – this may indicate infection or non-sexually transmitted causes including cervical ectropion, infection, cervical dysplasia
- Post-menopausal – causes include malignancy, vaginal atrophy and use of HRT
Abdominal or Pelvic Pain
Use the acronym SOCRATES to elicit the key features of any abdominal or pelvic pain:
Site
Onset
Character
Radiation
Associations
Time course
Exacerbating and relieving factors
Severity
Vaginal Discharge
Vaginal discharge is most often a normal and regular occurrence. However, a change in the character of discharge can indicate infection. Inquire about:
- Color
- Consistency
- Amount
- Smell
By TeachMeSeries Ltd (2025)
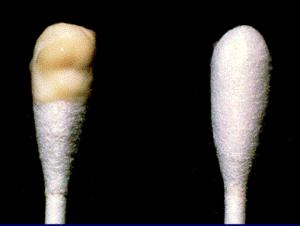
Fig 1 – Mucopurulent cervical discharge may be found in some sexually transmitted infections e.g. Chlamydia.
Other Symptoms
- Dyspareunia – pain during sexual intercourse. This can be divided into superficial or deep pain.
- Vulval itching and/or anogenital skin changes
- Infertility –inquire about duration, whether any investigations have been performed, and whether assisted conception has been attempted. Consider PID.
As part of the sexual history it is important to remember systemic and extragenital symptoms can be associated with STIs e.g. anal discharge, fever, urinary symptoms, joint pain and eye symptoms.
For males, it is important to ask about pain in the testes/scrotum, itching, skin changes, discharge, dysuria and systemic symptoms.
Menstrual History
A guide to taking a full menstrual history can be found in our gynaecological history article. When taking a sexual history the major menstrual symptom that may indicate infection is a change in bleeding e.g. new menorrhagia.
Acute Presentation
With acute or severe presentations is vital to exclude ectopic pregnancy and pelvic inflammatory disease in females and testicular torsion in males as these are medical emergencies.
Sexual Contact History
- Is the patient currently in a relationship?
- How long for?
- Is the relationship a sexual relationship?
- Contraception:
- Type
- Consistency
- Problems e.g. condom split
- Timing of last sexual contact
- Partners in the last 3 months:
- Number
- Genders
- Known infections
- For each sexual partner:
- Is the partner male/female?
- Nature of relationship? (regular, casual, paid, etc)
- Was it consensual – be aware of safeguarding issues
- When did you last have sex with him/her?
- What type of sex? (oral/anal/vaginal etc)
- Did you use condoms? Any other contraception?
- Did the condom break/fall off?
- Did the partner have any symptoms of an STI?
- What are the partner’s details? (name, region, age etc) – for contact tracing if appropriate
For the sexual contact history you might need to explain different terms to the patient e.g. active vs passive or insertive vs receptive.
Past Medical History
- Previous sexually transmitted infections (including in partners)
- Previous STI screens including HIV tests
- Cervical smears – the date of the last smear, its result and any treatments arising
- Previous gynaecological problems
- Surgical history – particularly any pelvic or abdominal surgery
- Pregnancies (a full obstetric history can be found here)
- Other medical conditions
Drug History

Fig 2 – An unrolled male condom. Contraceptive use is a key part of the sexual history.
- Contraception – note some medicines may reduce the effectiveness of the contraceptive pill
- Type and brand name
- Correct use
- Previous contraception history
- Hormone replacement therapy
- Recent antibiotic use – some antibiotics are associated with vaginal candidiasis and may inhibit growth of gonorrhea on culture media
- Allergies
Social History
In addition to smoking and alcohol it is important to ask about recreational drug use as IV drug users are at an increased risk of contracting hepatitis and HIV.
Assessing Blood-Borne Infection Risk
After taking a thorough sexual history it may be apparent that an individual is at an increased risk of having/contracting/transmitting HIV and other blood-borne infections such as syphilis, HBV and HCV. Positive risk factors include:
- Sexual contact with an HIV positive partner
- Engaging in sexual activities with a bisexual/homosexual man (explain term MSM)
- Engaging in sexual activities with someone from an area of high HIV prevalence
- IV drug use in patient/partner
- Paying/being paid for sex
- Receiving blood transfusions/tattoos/piercings in environments where sterile equipment cannot be guaranteed
Summary
Summarise throughout the history to check your understanding and ask the patient if there is anything they would like to add or discuss. It is also important to check with the patient their ideas, concerns and expectations i.e. what are their thoughts on their symptoms, any worries they may have and what they hope to gain from seeking medical advice.
For more information see our articles on sexually and non-sexually transmitted infections.
