Cervical ectropion occurs when there is eversion of the endocervix, exposing the columnar epithelium to the vaginal milieu. It is also known as a cervical erosion, although no “erosion” of cells actually occurs.
It is a normal physiological condition, which is commonly seen on examination of the cervix in adolescents, in pregnancy, and in women taking oestrogen containing contraceptives.
In this article, we shall look at the clinical features, investigations and management of cervical ectropion.
Aetiology and Pathophysiology
The cervix is the lower portion of the uterus. It is composed of two regions; the ectocervix and the endocervical canal.
- Endocervical canal (endocervix) – the more proximal, and ‘inner’ part of the cervix. It is lined by a mucus-secreting simple columnar epithelium.
- Ectocervix – the part of cervix that projects into the vagina. It is normally lined by stratified squamous non-keratinised epithelium.
A cervical ectropion is the presence of everted endocervical columnar epithelium on the ectocervix. This change is thought to be induced by high levels of oestrogen, and does not represent metaplasia.
The columnar epithelium contains mucus-secreting glands, and thus some individuals with cervical ectropion experience increased vaginal discharge. It may also give rise to post-coital bleeding, as the fine blood vessels present within the epithelium are easily broken during intercourse.
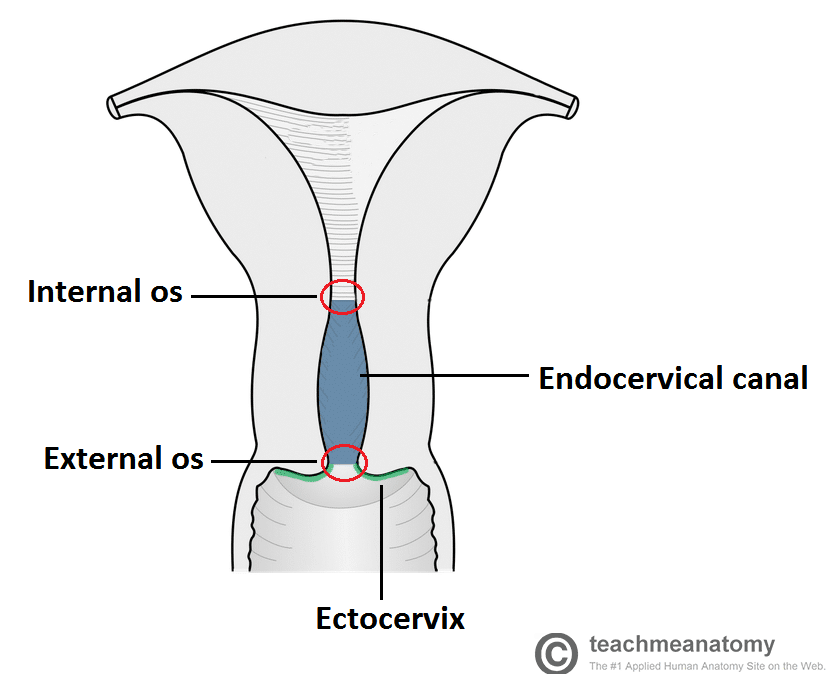
Fig 1 – The cervix can be divided into the endocervical canal and the ectocervix.
Risk Factors
It is thought that cervical ectropion is induced by high levels of oestrogen. Therefore, factors that increase the risk of ectropion are related to those that increase levels of oestrogen:
- Use of the combined oral contraceptive pill
- Pregnancy
- Adolescence
- Menstruating age (it is uncommon in post-menopausal women)
Clinical Features
Cervical ectropion is most commonly asymptomatic. It can occasionally present with post-coital bleeding, intermenstrual bleeding, or excessive discharge (non-purulent).
On speculum examination, the everted columnar epithelium has a reddish appearance – usually arranged in a ring around the external os.
Differential Diagnosis
In cases of suspected cervical ectropion, other diagnoses to consider are cervical cancer, cervical intraepithelial neoplasia, cervicitis (inflammation of the cervix, typically caused by infection), and pregnancy. These should be excluded using relevant investigations.
Investigations
Cervical ectropion is a clinical diagnosis. The main role of any investigation is to exclude other potential diagnoses:
- Pregnancy test
- Triple swabs – if there is any suggestion of infection (such as purulent discharge), endocervical and high vaginal swabs should be taken.
- Cervical smear – to rule out cervical intraepithelial neoplasia. If a frank lesion is observed, a biopsy should be taken (note that biopsies are not performed as routine).
Management
Cervical ectropion is regarded as a normal variant, and does not require treatment unless symptomatic.
First-line treatment is to stop any oestrogen containing medications – most commonly the combined oral contraceptive pill. This is effective in the majority of cases.
If symptoms persist, the columnar epithelium can be ablated, typically using cryotherapy or electrocautery. This will result in significant vaginal discharge until healing is completed.
Medication to acidify the vaginal pH has been suggested, such as boric acid pessaries.

