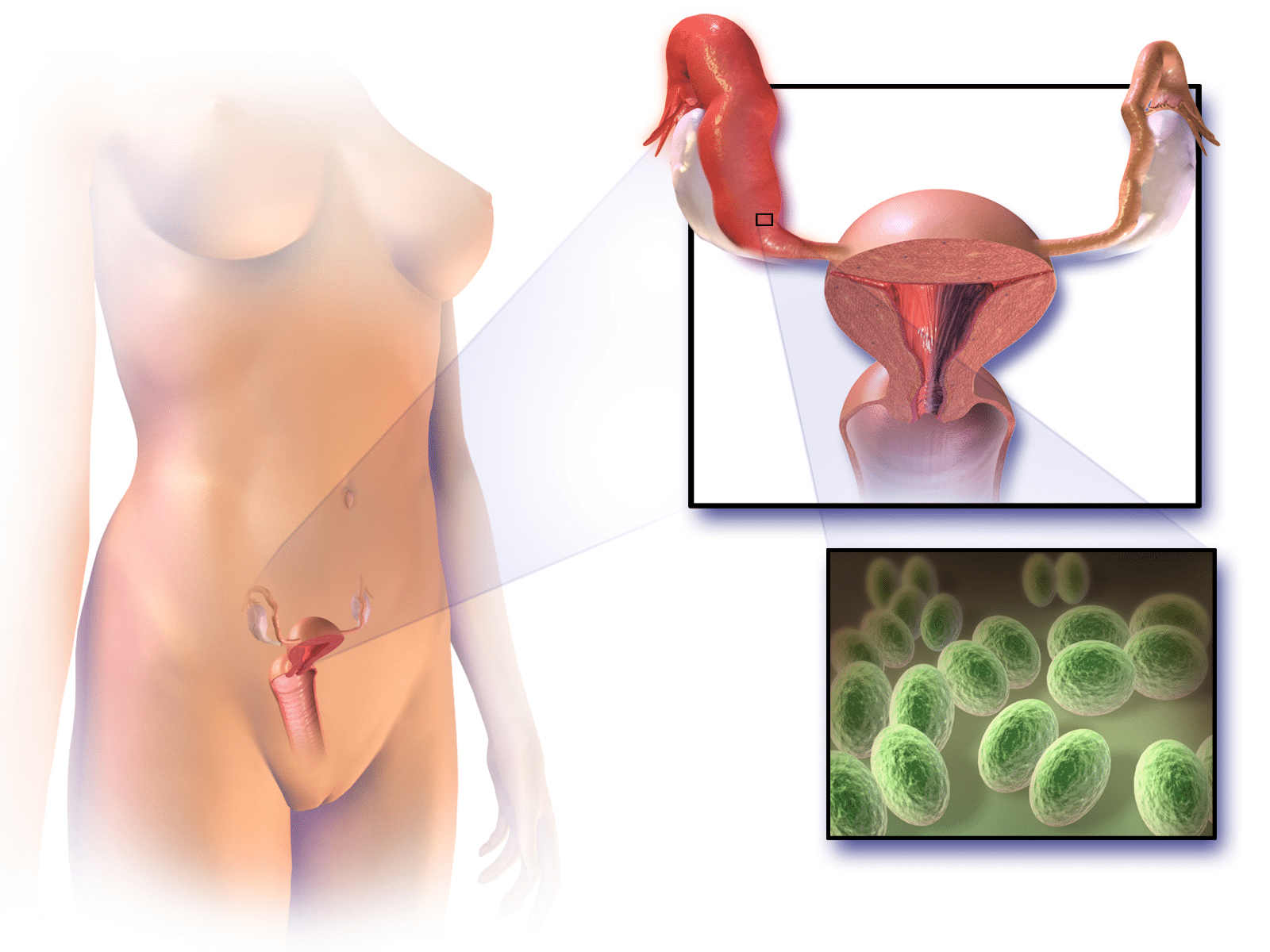
Dysmenorrhoea or “painful periods” is the most common of all gynaecological symptoms. It is generally described as a crampy lower abdominal pain, which starts at the onset of menstruation.
It can be classified as either:
- Primary – menstrual pain occurring with no underlying pelvic pathology.
- Secondary – menstrual pain that occurs with an associated pelvic pathology.
In this article, we shall look at the risk factors, clinical features and management of primary dysmenorrhoea.
Aetiology & Pathophysiology
In the absence of fertilisation of the egg, the corpus luteum regresses, and there is a subsequent decline in oestrogen and progesterone production.
The endometrial cells are sensitive to this decline in progesterone, and respond with prostaglandin release. Prostaglandins have two main actions in the uterus:
- Spiral artery vasospasm – leading to ischaemic necrosis and shedding of the superficial layer of the endometrium.
- Increased myometrial contractions.
Primary dysmenorrhoea is thought to occur secondary to the excessive release of prostaglandins (PGF2α and PGE2) by endometrial cells.
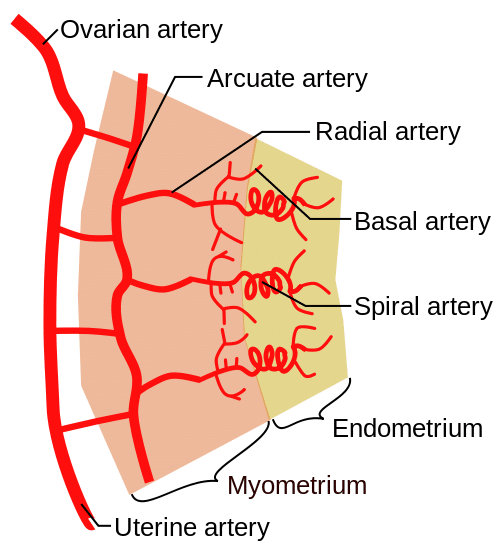
Fig 1 – Vasculature of the endometrium. The spiral arteries undergo vasospasm in response to prostaglandins.
Risk Factors
The risk factors for primary dysmenorrhoea include:
- Early menarche
- Long menstrual phase
- Heavy periods
- Smoking
- Nuliparity
Clinical Features
The typical description of dysmenorrhoea is lower abdominal or pelvic pain, which can radiate to lower back or anterior thigh.
Pain is crampy in nature. It usually lasts for 48-72 hours around the menstrual period, and is characteristically worst at the onset of menses.
The pain can be associated with other symptoms, such as; malaise, nausea, vomiting, diarrhoea, dizziness.
Abdominal and pelvic examinations (including speculum examination of cervix) are performed but are usually unremarkable. Uterine tenderness may be present.
Note: Dysmenorrhoea may resolve following pregnancy.
Differential Diagnosis
Primary dysmenorrhoea is a diagnosis of exclusion. Therefore, other diagnoses to consider are the main causes of secondary dysmenorrhoea:
- Endometriosis
- Adenomyosis
- Pelvic inflammatory disease
- Adhesions
Non-gynaecological differentials include inflammatory bowel disease and irritable bowel syndrome.
Investigations
No investigations are specific to primary dysmenorrhoea and therefore the work up is focused on ruling out underlying pathology.
If the patient is at high risk of a sexually transmitted infection, then a high vaginal swab and endocervical swabs are indicated to screen for underlying infection.
If on examination a pelvic mass is palpated, a transvaginal ultrasound scan (TVS) should be performed to investigate further.
Management
As there is no pathology to treat in primary dysmenorrhoea, the aim is a symptomatic improvement.
This can be achieved by lifestyle changes, pharmacological therapy and/or non-pharmacological measures:
Lifestyle Changes
- Stop smoking (there is a clear relationship between smoking and dysmenorrhoea).
Pharmacological
- Anagelsia (First line):
- NSAIDs (ibuprofen, naproxen, mefenamic acid). They work by inhibiting the production of prostaglandins; which have been implicated in the pathogenesis of primary dysmenorrhoea.
- And/or paracetamol
- 3-6 month trial of hormonal contraception (Second line):
- Monophasic combined oral contraceptive pill is most commonly used first line.
- Intrauterine system (e.g Mirena coil) may also be effective.
Non-Pharmacological
- Local application of heat (water bottles or heat patch)
- Transcutaneous Electrical Nerve Stimulation (TENS)
Summary
- Primary dysmenorrhoea refers to menses pain in the absence of an underlying pelvic pathology.
- Prostaglandins released stimulate myometrial contraction and spiral artery vasospasm causing ischaemia of the secretory layer of the endometrium.
- It typically has a good response to COCP and NSAID therapy.