Placenta praevia is where the placenta is fully or partially attached to the lower uterine segment. It is an important cause of antepartum haemorrhage – vaginal bleeding from week 24 of gestation until delivery.
In this article, we shall look at the pathophysiology, clinical features and management of placenta praevia.
Pathophysiology
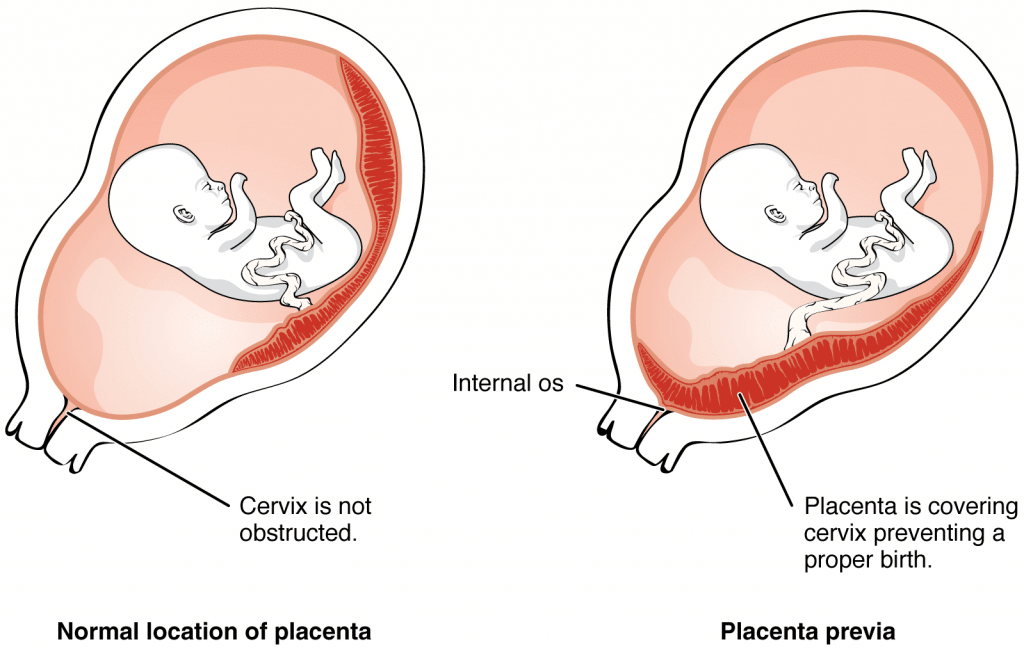
Placenta praevia is where the placenta is fully or partially attached to the lower uterine segment. There are two main types:
- Minor placenta praevia – placenta is low but does not cover the internal cervical os.
- Major placenta praevia – placenta lies over the internal cervical os.
A low-lying placenta is more susceptible to haemorrhage, possibly due to a defective attachment to the uterine wall. Bleeding can be spontaneous, or provoked by mild trauma (e.g vaginal examination). Additionally, the placenta may be damaged as the presenting part of the fetus moves into the lower uterine segment in preparation for labour.
Risk Factors
The main risk factor for placenta praevia is previous caesarean section. There is a 1 in 160 incidence associated with 1 previous section – this rises to 1 in 60 with 2 previous sections, to 1 in 10 with 4 sections.
The other risk factors include:
- High parity
- Maternal age >40 years
- Multiple pregnancy
- Previous placenta praevia
- History of uterine infection (endometritis)
- Curettage to the endometrium after miscarriage or termination
Clinical Features
Any woman presenting with antepartum haemorrhage (APH) should be assessed in a systematic manner (see box below).
Placenta praevia classically presents as painless vaginal bleeding, this can vary between spotting to massive haemorrhage. There can be pain if the woman is in labour.
Examination may reveal risk factors pertinent to placenta praevia – e.g. c-section scar or multiple pregnancy. The uterus is usually not tender on palpation.
Assessment of Antepartum Haemorrhage
History
The following questions are useful to ask in the assessment of antepartum haemorrhage:
- How much bleeding was there and when did is start?
- Was it fresh red or old brown blood, or was it mixed with mucus?
- Could the waters have broken (membranes ruptured?)
- Was it provoked (post-coital) or not?
- Is there any abdominal pain?
- Are the fetal movements normal?
- Are there any risk factors for abruption? e.g. smoking/drug use/trauma – domestic violence is an important cause.
If the bleed is ongoing, or if there has been a significant vaginal bleed, ABC assessment and resuscitation is vital. If the woman is clinically stable, proceed to examination.
General Examination
On general examination, the following should be assessed:
- Pallor, distress, check capillary refill, are peripheries cool?
- Is the abdomen tender?
- Does the uterus feel ‘woody’ or ‘tense’ (which may indicate placental abruption)?
- Are there palpable contractions?
- Check the lie and presentation of the fetus/fetuses. Ultrasound can be used to help.
- Check fetal wellbeing with a cardiotocograph (CTG) at 26 weeks gestation or above: (otherwise auscultate the fetal heart only).
- Read the hand-held pregnancy notes: are there scan reports? This will be helpful in establishing whether there could be placenta praevia
Assessment of Bleeding
Lastly, the bleeding itself should be assessed:
- Externally e.g. by looking at pads.
- Cusco speculum examination: avoid this until placenta praevia has been excluded by USS.
- Look for whether blood is fresh red or dark. How much blood is there? Are there clots? Are there any cervical lesions? Is there any cervical dilatation, or any chance that the membranes have ruptured?
- Take triple genital swabs to exclude infection if the bleeding is minimal
- Digital vaginal examination: A digital vaginal examination with known placenta praevia should NOT be performed as it could cause massive bleeding.
- In minor bleed, when placenta praevia is excluded, it can help to establish whether the cervix is beginning to dilate.
- Avoid digital VE if the membranes have ruptured.
Differential Diagnoses
Placenta praevia is an important cause of antenatal haemorrhage; but it is not the most common. Differential diagnoses to consider include:
- Placental abruption – where a part or all of the placenta separates from the wall of the uterus prematurely.
- Vasa praevia – where fetal blood vessels run near the internal cervical os. It is characterised by a triad of (i) Vaginal bleeding; (ii) Rupture of membranes; and (iii) Fetal compromise.
- The bleeding occurs following membrane rupture when there is rupture of the umbilical cord vessels, leading to loss of fetal blood and rapid deterioration in fetal condition.
- Uterine rupture – a full-thickness disruption of the uterine muscle and overlying serosa. This usually occurs in labour with a history of previous caesarean section or previous uterine surgery such as myomectomy.
- Local genital causes:
- Benign or malignant lesions – e.g. polyps, carcinoma. cervical ectropion (common).
- Infections – e.g. candida, bacterial vaginosis and chlamydia.
Investigations
If major bleeding is suspected, resuscitate and perform investigations simultaneously.
Haematology
- Full blood count – assess any maternal anaemia.
- Clotting profile
- Kleihauer test – if the woman is Rhesus negative (to determine the amount of feto-maternal haemorrhage and thus the dose of Anti-D required).
- Group and Save – if blood group is unknown.
- Cross-match – if the clinical presentation is likely to warrant transfusion.
Biochemistry
These are performed to exclude hypertensive disorders including pre-eclampsia and HELLP syndrome, and any other organ dysfunction:
- Urea and electrolytes
- Liver function tests
Assess Fetal Wellbeing
In women above 26 weeks gestation, a cardiotocograph (CTG) should be performed to assess fetal wellbeing.
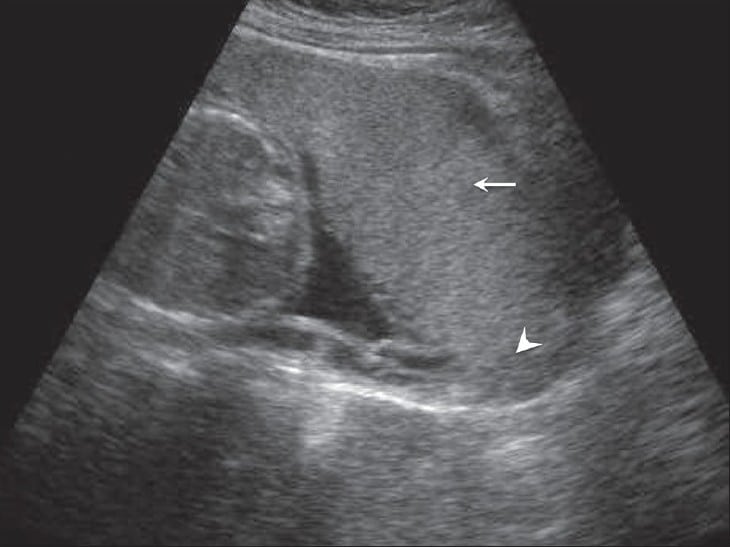
Imaging
The definitive diagnosis of placenta praevia is via ultrasound. There is a short distance between the lower edge of the placenta and internal os.
Management
Any woman presenting with a significant antepartum haemorrhage should be resuscitated using an ABCDE approach. Do not delay maternal resuscitation in order to determine fetal viability.
Placenta praevia may be identified in an asymptomatic patient at their 20-week ultrasound scan:
- Placenta praevia minor – a repeat scan at 36 weeks is recommended, as the placenta is likely to have moved superiorly.
- Placenta praevia major – a repeat scan at 32 weeks is recommended, and a plan for delivery should be made at this time.
In cases of confirmed placenta praevia, Caesarean section is the safest mode of delivery. Placenta praevia major usually warrants an elective Caesarean section at 38 weeks.
In all cases of antepartum haemorrhage, give anti-D within 72 hours of the onset of bleeding if the woman is rhesus D negative.