Syphilis is a sexually transmitted infection caused by the spirochete gram-negative bacterium Treponema pallidum subspecies pallidum. In the UK, there were over 5,000 cases of syphilis diagnosed in 2015 and incidence is increasing, particularly in high-risk groups such as men who have sex with men (MSM).
Other subspecies of Treponemes are responsible for non-sexually transmitted diseases such as Bejel, a chronic skin and tissue disease, Yaws, a disease of the bones and joints, and Pinta, a skin disease. Unlike syphilis, these diseases are transmitted by any close contact (sexual or not) and do not pass from mother to fetus.
In this article we shall consider the pathophysiology, clinical features and management of syphilis and also how it may affect pregnancy.
Pathophysiology
In addition to sexual transmission, the infection can also be transmitted from mother to fetus via the placenta (congenital syphilis) and through infected blood products.
The motile Treponema pallidum enters through a break in the skin or through intact mucous membranes. The bacteria divide and an infectious hard ulcer (chancre) subsequently forms at the site of contact after an incubation period of 2-3 weeks. This is the first stage of acquired symptomatic syphilis: primary syphilis.
If left untreated, T. pallidum can persist and cause systemic damage via obliterating arteritis. This is where endothelial cells of the vessels excessively proliferate causing the lumen of the vessels to become narrowed. This can then result in ischaemia at the tissues supplied by these arteries which leads to the symptoms associated with syphilis.
Risk factors
- Engaging in unprotected sex – especially with high risk partners.
- Multiple sexual partners.
- Men who have sex with men (MSM).
- HIV infection.
Clinical Features
Syphilis is divided into congenital and acquired. Acquired syphilis is further divided into early (2 years since infection). Acquired syphilis can be asymptomatic (latent) or symptomatic, which can be primary, secondary or tertiary (cardiovascular, neurological or gummatous).

Fig 2. A chancre located on the shaft of the penis.
Primary syphilis
Following inoculation, a papule (slightly elevated lesion with no fluid) will appear before ulcerating into a chancre. A chancre is a painless ulcer and typically develops 9-90 days post infection on a genital site e.g. penis, scrotum, anus, rectum, labia or cervix. As well as painless, they are usually singular, hard and non-itchy. However, chancres may be atypical in that they can appear at other sites e.g. oral, be multiple and painful. Classically chancres heal within 3-10 weeks with or without symptoms but may persist during secondary syphilis.
Secondary syphilis
Secondary syphilis usually develops 3 months post infection. Signs and symptoms include:

Fig 3. Rash typical of secondary syphilis
- Skin rash – hands and soles of the feet (not usually itchy or painful)
- Fever
- Malaise
- Arthralgia
- Weight loss
- Headaches
- Condylomata lata- elevated plaques like warts at moist areas of skin e.g. inner thighs, anogenital region, axillae
- Painless lymphadenopathy
- Silvery-gray mucous membrane lesions – oral, pharyngeal, genital
There are many other manifestations of secondary syphilis e.g. affecting the kidneys, liver and brain. Following secondary syphilis, the disease then enters the asymptomatic latent phase.
Tertiary syphilis
Tertiary disease can present many years after the initial infection and can be categorised into gummatous syphilis, neurosyphilis and cardiovascular syphilis.
Gummatous syphilis:
Granulomas can form in bone, skin, mucous membranes of the upper respiratory tract, mouth and viscera or connective tissue e.g. lung, liver, testis. Patients at this stage are non-infectious. Signs and symptoms vary according to the tissue affected.
Neurosyphilis:
- Tabes dorsalis – ataxia, numb legs, absence of deep tendon reflexes, lightning pains, loss of pain and temperature sensation, skin and joint damage.
- Dementia – cognitive impairment, mood alterations, psychosis.
- Meningovascular complications – cranial nerve palsies, stroke, cerebral gummas.
- Argyll Robertson pupil – pupil is constricted and unreactive to light, but reacts to accommodation.
Cardiovascular syphilis:
- Aortic regurgitation due to aortic valvulitis (diastolic murmur), also aortic root dilatation.
- Angina due to stenosis of the coronary ostia.
- Dilation and calcification of the ascending aorta.
Investigations
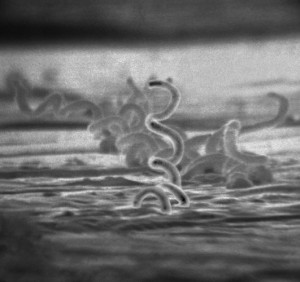
- Dark ground microscopy of chancre fluid- detects spirochaete in primary syphilis
- PCR testing of swab from active lesion
- Serology:
- Treponemal tests – assess for exposure to treponemes (NB not necessarily syphilis)
- Treponemal ELISA (IgG/IgM) – remains positive for life
- TPPA or TPHA – remain positive for life
- Non-treponemal tests:
- RPR/VDRL: rises in early disease; falling titres indicate successful treatment or progression to late disease. False positives can occur in inflammatory conditions or during pregnancy.
- Treponemal tests – assess for exposure to treponemes (NB not necessarily syphilis)
- Lumbar puncture: CSF antibody tests in neurosyphilis
Management
Penicillin is the treatment of choice. Patients with penicillin allergy should be considered for desensitisation. As Treponema pallidum ssp pallidum replicates slowly, prolonged courses of antibiotics are required for late disease.
First line treatment for syphilis:
- Early syphilis: Benzathine penicillin 2.4 MU IM single dose.
- Late syphilis: Benzathine penicillin 2.4 MU IM 3 doses at weekly intervals.
Neurosyphilis (at any stage, including ophthalmic syphilis):
- Procaine penicillin 1.8 MU–2.4 MU IM OD plus probenecid 500 mg PO QDS for 14 Days or Benzylpenicillin 10.8–14.4 g daily, given as 1.8–2.4 g IV every 4 h for 14 days:
Recommended regimes for each stage of syphilis can be found at the British Association for Sexual Health and HIV (BASHH) website.
Management also comprises:
- Advising patients to avoid sexual contact of any kind, or exposure of other people to active lesions until the condition has been successfully treated
- Screening for other STIs
- Patient education
- Contact tracing
- Follow-up serology to determine response to treatment
The Jarisch Herxheimer reaction is an inflammatory response secondary to death of treponemes, and results in a flu-like illness within 24 hours of treatment. Supportive measures are all that is required, unless a patient has cardiovascular or neurosyphilis, in which case oral steroids should be administered prior to antibiotics to reduce the risk of an acute localised inflammatory reaction.
Syphilis in Pregnancy
Pregnant women in the UK are offered antenatal screening for syphilis, HIV and hepatitis B at their first antenatal appointment. T. pallidum has the potential to cross the placenta or infect the baby during delivery. It is important to treat pregnant women early to reduce the risk of adverse outcomes. If left untreated, syphilis during pregnancy may result in miscarriage, stillbirth, pre-term labour or congenital syphilis. Congenital syphilis is typically severe and debilitating and may present with saddle nose, rashes, fever and failure to gain weight. Full BASHH guidelines for management during pregnancy can be found here.