A gynaecological history is an assessment of the female reproductive system.
It can be a delicate subject for some women, and it is important to treat any information divulged with sensitivity and respect. However, the clinician cannot shy away from asking clinically relevant questions.
The history should be tailored to the specific presenting complaint(s), but a generic outline would involve structured and systematic approach – as described below.
Gynaecology History in the Emergency Setting
In an emergency scenario, a focused history may be more appropriate. This is best described by the acronym SAMPLE:
- Signs/Symptoms
- Allergies
- Medication
- Past illness/Pregnancy
- Last oral intake
- Events leading to current clinical picture
History of Presenting Complaint
First, use open questioning to allow the patient to fully elaborate on their presenting problem. Ask about impact on their daily life, and how it is currently being managed.
The specific details to elicit from the presenting complaint include:
- Type and site of symptoms
- Timing:
- Onset and duration
- Cyclical – are symptoms associated with menstruation?
- Intermittent or continuous
- Exacerbating and relieving factors
- Previous episodes – including any investigations and treatments
- Other associated symptoms
Gynaecological Symptoms
After exploring the history of presenting complaint, a thorough gynaecology history should inquire about the common symptoms of gynaecological disease. These include:
Vaginal Bleeding
Abnormal vaginal bleeding exists in three main forms:
- Intermenstrual (between menstrual periods) – causes include infection, malignancy, fibroids, endometriosis, pregnancy, and hormonal contraception.
- Post-coital (after sexual intercourse) – causes include cervical ectropion, infection, vaginitis, and malignancy.
- Post-menopausal (after the menopause) – causes include malignancy, vaginal atrophy, and use of hormone replacement therapy.

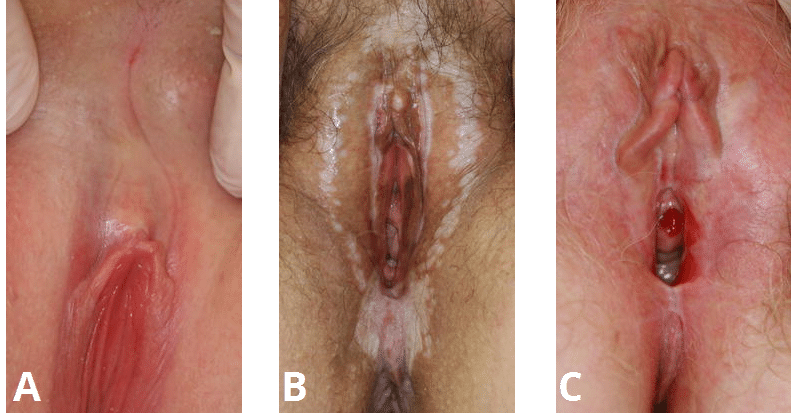
Fig 1 – Cervical ectropion on speculum examination. Ectropion in a common cause of post-coital bleeding.
Abdominal or Pelvic Pain
Use the acronym SOCRATES to elicit the key features of any abdominal or pelvic pain:
- Site
- Onset
- Character
- Radiation
- Associations
- Time course
- Exacerbating and relieving factors
- Severity
Vaginal Discharge
Vaginal discharge is most often a normal and regular occurrence. However, a change in the character of discharge can indicate infection. Inquire about:
- Color
- Consistency
- Amount
- Smell
Menstrual History
A menstrual history is a key part of any gynaecological assessment. It has the following components:
- Frequency – average 28 days
- <24 days Frequent, >38 days Infrequent
- Duration – average 5 days
- >8 days Prolonged, <4.5 days shortened
- Volume – average 40ml menstrual blood loss over course of menses
- >80ml heavy (Hb and Ferritin affected), <5ml Light
- Women may describe ‘flooding’ and clots passed
- Date of last menstrual period (LMP)
- If late, consider performing a pregnancy test.
If postmenopausal, record the date of the menopause.
Other Symptoms
- Dyspareunia – pain during sexual intercourse. This can be divided into superficial or deep pain.
- Vulval itching and/or anogenital skin changes.
- Infertility – inquire about duration, whether any investigations have been performed, and whether assisted conception has been attempted.
Past Medical History
The past medical history is an important aspect of gynaecological history taking. In particular, inquire about:
- Pregnancies (learn about a full obstetric history here):
- Number of births/miscarriages/abortions/ectopics.
- Means of delivery, age of child and birth weight.
- Explore any obstetric/delivery complications.
- Cervical smear – ascertain the date of the last smear, its result, and any treatment arising.
- Surgical history – particularly any pelvic or abdominal surgery.
- Previous gynaecological problems
- Previous sexually transmitted infections
Drug History
Many prescribed (and over the counter) medications can have an effect on gynaecological health. Inquire about the use of the following:
- Contraception:
- Type and brand name
- Correct use
- Previous contraception history
- Hormone replacement therapy:
- Duration of use
- Cyclical or continuous
- Combined or oestrogen-only
- Method of delivery.
- Recent antibiotic use – some antibiotics are associated with vaginal candidiasis.
- Any other medications – including over the counter medications
- Known allergies
Family History
A family history of any of the following is particularly relevant in a gynaecological history:
- Breast/ovarian cancer/endometrial cancer – can be familial (e.g BRCA 1/2 gene).
- Diabetes – associated with some reproductive abnormalities.
- Bleeding disorders – can be associated with menorrhagia.
Social History
The social history is an important part of a gynaecological history. In many cases, the patient’s lifestyle can influence disease and/or symptomatology:
- Weight:
- Rapid weight loss can cause oligo/amenorrhoea.
- Obesity can cause menstrual changes, and increase the risk of endometrial cancer.
- Occupation – some industrial exposures are risk factors for gynaecological disease.
- Home situation – who is at home? Are they independent? These are crucial when planning treatment.
- Smoking and alcohol intake
- Diet and exercise
Systems Review
Systemic symptoms can be related to gynaecological disease (and vice-versa). Therefore, a full systems review is needed in the gynaecological history.
Particularly relevant features include urinary symptoms, bowel symptoms, fever (e.g. PID), fatigue (e.g. menorrhagia associated anaemia), weight loss (e.g. malignancy) and abdominal distension (malignancy).
Summary
Use the summary to check your understanding of the problem, and prompt the patient to volunteer any other information they think might be relevant.
It is also important (particularly in the exam setting) inquire about the patient’s ideas, concerns and expectations (ICE) – this can guide you when discussing the next steps.