Barrier contraception is one of the most common forms of contraception used in the UK. Barrier contraception prevents pregnancy by stopping the male’s sperm from coming into contact with the female’s ovum. Depending on the type of contraception, they may convey a decreased risk of STI transmission.
In this article, we will explore the various types of barrier contraception, their benefits, drawbacks and efficacy rates.
Types of barrier contraception
Principally, there are four physical barrier contraceptive types:
- Male condoms – typically made of latex, male condoms are rolled down from the tip of the penis to the base. Semen collects in a reservoir at the tip end of the condom. They are proven to reduce transmission of many STIs such as chlamydia and gonorrhoea.
- Female condoms – made of polyurethane, these are tubular shaped, where an inner ring sits deep in the vagina, with an open outer ring sitting just outside the vulva. The male inserts their penis into the female condom, preventing contact with the vagina. They are proven to reduce transmission of many STIs, such as chlamydia and gonorrhoea.
- Diaphragms – these are typically rubber structures with a metal inner frame that spans the posterior fornix to the anteroinferior wall of the vagina, covering the cervix and therefore preventing entry of semen. They are held in place by a combination of vaginal tone, the rigid metal inner frame and the pubic symphysis. Often combined with spermicide to increase their efficiency.
- Cervical caps – these sit directly over the cervix, and are held in place by suction and vaginal tone. They are often combined with spermicide to increase their efficiency.
- As these have the same advantages and disadvantages as diaphragms they shall be considered together in this article.
Advantages
Male condom
- Not contraindicated by any condition exception latex allergy, in which other materials (such as polyurethane) can be used, with similar efficiency rate.
- It is the only contraceptive method mentioned that is controlled by the male, which may be desirable by the couple.
- Widely available and simple to use, and only need to be used immediately before intercourse.
- Are protective against many STIs.
Female condom
- No contraindications.
- Less likely to tear than the male condom.
- May protect against some STIs.
- Can be inserted up to 8 hours before intercourse.
Diaphragm/cap
- Can be inserted up to 3 hours before intercourse.
Disadvantages
Male condom
- Perfect use is rarely achieved – may tear or couple may lack motivation to use them every time.
- Can reduce sensitivity and/or arousal.
Female condom
- Perfect use is rarely achieved – may become dislodged or couple may lack motivation to use them every time.
- Penis may be inserted between condom and vaginal wall.
- Can be noisy and/or uncomfortable for the woman during intercourse.
Diaphragm/cap
- Perfect use is rarely achieved – may tear or couple may lack motivation to use them every time.
- They require prior planning and careful insertion.
- They require measuring and fitting to find the correct size – any weight gain or pregnancy mandates a refitting.
- They are associated with a higher risk of urinary tract infections.
- Most likely due to the position of the diaphragm/cap putting pressure on the urethra.
- STI transmission is not reduced – in fact spermicide may irritate vaginal mucosa, possibly increasing the rate of transmission.
Failure rates
Failure rates for barrier contraception are much higher than those of long acting reversible contraception. These methods require thought at intercourse hence their typical and perfect use failure rates vary greatly. All values are expressed as the percentage of women who will get pregnant in one year using this method.
| Perfect Use | Typical Rate | |
| Male Condoms | 2% | 16% |
| Female Condoms | 5% | 21% |
| Diaphragm | 6% | 16% |
| Cervical Cap: Nulliparous | 9% | 16% |
| Cervical Cap: Parous | 20% | 32% |
Points to consider
- All patients should be offered verbal and/or written advice on long acting reversible contraception, due to their lower failure rates.
- Male condoms protect against STIs (as do female condoms to a lesser degree) – they are the only type of contraception to offer this protection.
- Contraception may be provided to under 16s provided they meet the Fraser criteria.
- Inform all patients of the limited efficacy of barrier methods versus long acting reversible methods.
- All patients should be aware of the need for emergency contraception (link) should barrier contraception fail or be omitted.



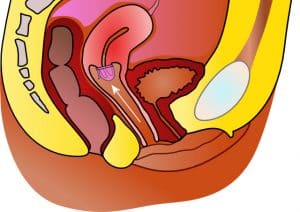
 Fig 2 A female condom. Note the two rings, one which sits deep in the vagina, and one that sits outside the vulva.[/caption]
Fig 2 A female condom. Note the two rings, one which sits deep in the vagina, and one that sits outside the vulva.[/caption]