There are around 37 million people in the world living with human immunodeficiency virus (HIV). HIV is a single stranded RNA retrovirus that infects and replicates within the human immune system using host CD4 cells.
Without treatment, destruction of the immune system can lead to acquired immune deficiency syndrome (AIDS).
In this article we shall look at the pathophysiology, clinical features, investigations and management of HIV.
Pathophysiology
HIV is a single stranded RNA retrovirus that infects and replicates with CD4 cells (T helper cells).
First, it penetrates the host CD4 cell and empties its contents. Single strands of the viral RNA are converted into double stranded DNA by reverse transcriptase, and combined with the host DNA using the enzyme integrase.
When the infected cell divides, the viral DNA is read, creating viral protein chains and the immature virus pushes out of the cell, retaining some cell membrane.
The virus matures when the protease enzyme cuts the viral protein chains, and they assemble to create a working virus. The host cell is destroyed during this process.
CD4 Levels
Upon seroconversion (the process of producing anti-HIV antibodies during primary infection), the patient may experience flu-like symptoms. CD4 levels fall in response to the initial, rapid replication of HIV – and at this stage a person is extremely infectious.
Over the next months-years the infection can enter a latent phase. The patient may initially be asymptomatic, but with CD4 levels falling and viral load increasing, they may become more susceptible to infections. The HIV infection can later become symptomatic and eventually, over an average of 10 years, develop into AIDS.
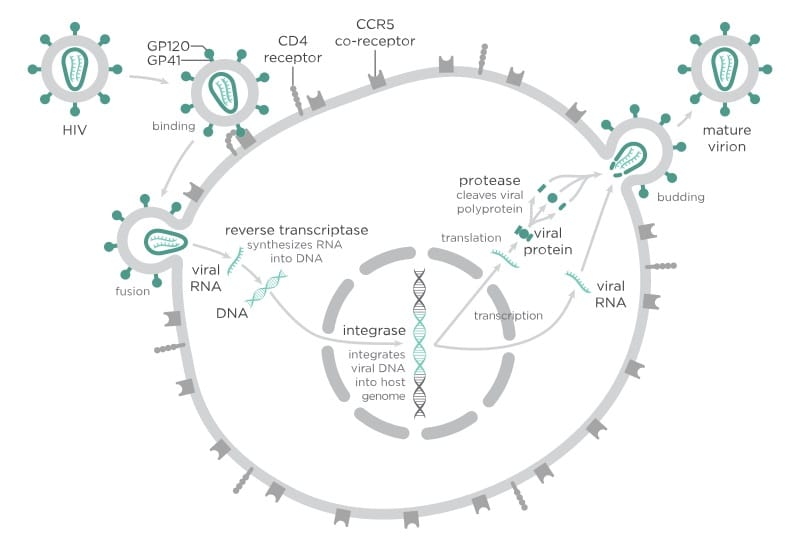
Fig 1 – The process of HIV infecting and reproducing within cells.
Transmission
HIV can be transmitted in the following ways:
- Unprotected sexual contact – vaginal, anal or oral.
- Sharing of injecting equipment.
- Medical procedures – blood products, skin grafts, organ donation and artificial insemination.
- Vertical transmission – from mother to child in utero, during childbirth or breast feeding.
People are more likely to catch HIV if they are exposed to a higher viral level, if they have sexually transmitted infections causing anogenital inflammation, or if they have any breaks in the skin or mucosa.
HIV is a preventable disease and practitioners need to be able to advise patients regarding transmission reduction and safer sex.
At-Risk Groups in the UK
Certain groups have a higher risk of becoming infected with HIV. The at-risk groups in the UK include:
- Men who have sex with men
- Intravenous drug users
- Those in high prevalence areas
- Those who have had unprotected sex with a partner who has lived or travelled in Africa
There is a need to encourage testing for those at risk and those with indicator conditions.
Clinical Features
The clinical features of HIV can be divided into the initial seroconversion illness and symptomatic HIV.
Seroconversion Illness
2-6 weeks after exposure, patients may experience a non-specific, flu-like illness. Features include:
- Fever
- Muscle aches
- Malaise
- Lymphadenopathy
- Maculopapular rash
- Pharyngitis
Over the next months-years the infection can enter a latent, asymptomatic phase.
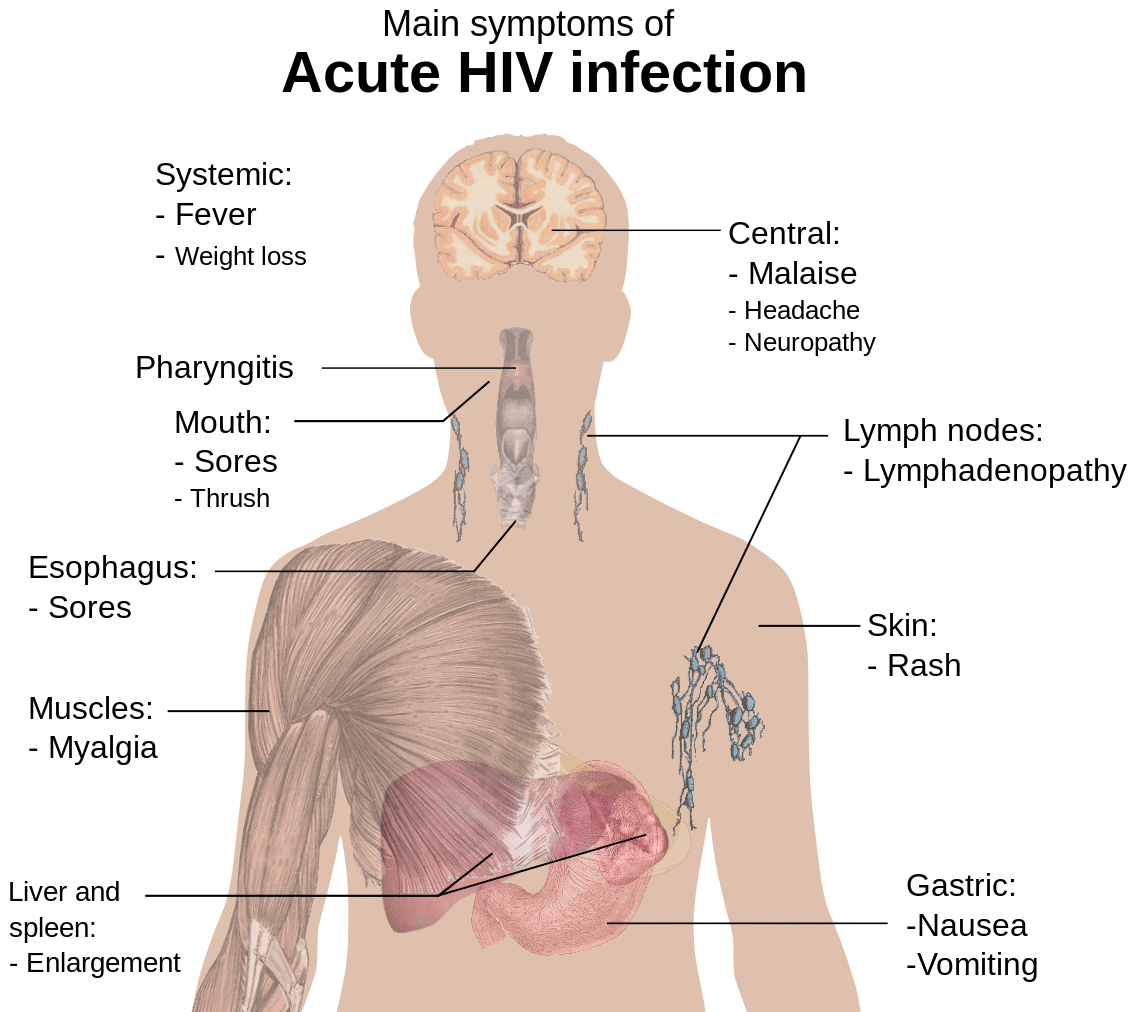
Fig 2 – Symptoms of the initial seroconversion illness (acute HIV infection).
Symptomatic HIV
After a latent phase, the HIV infection will become symptomatic. The patient may experience:
- Weight loss
- High temperatures
- Diarrhoea
- Frequent minor opportunistic infections, e.g. herpes zoster or candidiasis
AIDS-Defining illnesses
If left untreated, HIV can progress to AIDS. This is an advanced stage of the disease where the immune system is significantly weakened.
It is characterised by the development of certain (AIDS-defining) infections and malignancies, for example, pnuemocystis jiroveci pneumonia, non-Hodgkin’s lymphoma, and TB.
Investigations
Fourth-generation tests are the first line of investigation. These are ELISAs that test for serum (or salivary) HIV antibodies and p24 antigen. They normally give reliable results 4-6 weeks after exposure.
Other rapid test kits can give results in 30 minutes, and home-sampling kits and home-testing kits are available. However, these tests are less accurate and if positive, the diagnosis still needs to be confirmed by ELISA.
Contact tracing is also important to identify those at risk and prevent further spread of the disease.
Management
Highly active antiretroviral therapy (HAART) does not cure HIV, but aims to reduce the viral load to undetectable levels in the serum. With an undetectable load, people living with HIV have an excellent prognosis and risk of onward transmission of HIV is very small.
It is now recommended that all people with living with HIV should be treated with antiretroviral therapy, which significantly reduces the risk of AIDS-related and non-AIDS related mortality.
A number of classes of drugs including nucleoside reverse transcriptase inhibitors (NRTIs), protease inhibitors (PIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs) and integrase strand transfer inhibitors (InSTIs) are used in combination to target the enzymes used in viral replication and maturation.
Where possible, these drugs are combined into one tablet to be taken daily:
- Atripla: tenofovir + emtricitabine + efavirenz
- Stribild: elvitegravir + cobicistat + tenofovir + emtricitabine
- Eviplera: tenofovir + emtricitabine + rilpivirine
- Triumeq: abacavir + lamivudine + dolutegravir
Compliance is key and the patient must keep taking the drugs for the rest of their lives. Non-adherence to HAART can result in resistance mutations which make treatment difficult or impossible.
It is also important not to forget about managing the psychological impact of living with or being diagnosed with HIV.
Monitoring
In the monitoring of HIV, regular tests include:
- CD4 count
- HIV viral load
- FBC
- U&Es
- Urinalysis
- ALT, AST and bilirubin
Patients may also require pregnancy testing, and in treatment failure, resistance testing.
Post-Exposure Prophylaxis
If somebody has or suspects that they have been exposed to the virus within the last 72 hours they can commence post-exposure prophylaxis (PEP) to lower the risk of becoming infected.
A PEP course lasts for a month:
- Truvada (one tablet daily) + Raltegravir (one tablet twice daily)
HIV and Pregnancy
HIV can be transmitted in utero, at delivery and through breastfeeding. There are several measures that can be taken to reduce the risk of transmission:
- Antenatal antiretroviral therapy during pregnancy and delivery
- Avoidance of breastfeeding
- Neonatal post-exposure prophylaxis
Collectively, these interventions reduce the risk of HIV transmission to the baby to <1%. Without them, the risk of transmission is greater than 1 in 4. Caesarean birth is no longer routinely recommended if the mother has an undetectable viral load at delivery.

