An operative vaginal delivery (OVD) is defined as the use of an instrument to aid delivery of the fetus
In the UK, operative vaginal delivery rates have remained stable at 12-13%; yielding safe and satisfying outcomes for the majority of the women and babies [RCOG, 2011].
In this article, we shall look at the indications, classification, and pre-requisites for an operative vaginal delivery.
Instrument Types
There are two main instruments used in operative deliveries – the ventouse and the forceps.
In general, the first instrument used is the most likely to succeed. The choice is operator dependent, but forceps tend to have a lower risk of fetal complications, and a higher risk of maternal complications.
The general rule is, if after three contractions and pulls with any instrument there is no reasonable progress, the attempt should be abandoned.
Ventouse
The ventouse is an instrument that attaches a cup to the fetal head via a vacuum. There are many different systems used, but the most common are:
- An electrical pump attached to a silastic cup.
- This is only suitable if the fetus is in an occipital-anterior position.
- A hand-held, disposable device commonly known as the “Kiwi”.
- This is an omni-cup – it can be used for all fetal positions, and rotational deliveries.
There are also cups that can be used with the electrical pump that are suitable for OP positions. These are generally metal cups with the tubing attached to the side of the cup as opposed to the middle – the Bird cup.
To use the ventouse, the cup is applied with its centre over the flexion point on the fetal skull (in the midline, 3cm anterior to the posterior fontanelle). During uterine contractions, traction is applied perpendicular to the cup. Ventouse deliveries are associated with:
- Lower success rate
- Less maternal perineal injuries
- Less pain
- More cephalhaematoma
- More subgaleal haematoma
- More fetal retinal haemorrhage
Forceps
The forceps are double bladed instruments. Types include:
- Rhodes, Neville-Barnes or Simpsons – used for OA positions.
- Wrigley’s – used at Caesarean section.
- Kielland’s – used for rotational deliveries.
The blades are introduced into the pelvis, taking care not to cause trauma to maternal tissue, and applied around the sides of the fetal head, with the blades then locked together. Gentle traction is then applied during uterine contractions, following the J shape of the maternal pelvis. Use of the forceps is associated with:
- Higher rate of 3rd/4thdegree tears
- Less often used to rotate
- Doesn’t require maternal effort
Indications
The decision to perform an operative vaginal delivery should be based on the entire clinical scenario in the 2nd stage of labour. There are two questions that should be asked:
- Is there a valid clinical indication to intervene?
- Is the patient a suitable case for an instrumental delivery?
The most common indications for performing an operative vaginal delivery are listed below:
| Table 1 – Indications for Performing an Assisted Vaginal Delivery | |
| Maternal |
|
| Fetal |
|
Contraindications
Instrumental delivery is contraindicated if the risk to the mother or fetus is deemed unacceptable. Some examples include, but are not limited to:
Absolute:
- Unengaged fetal head in singleton pregnancies.
- Incompletely dilated cervix in singleton pregnancies.
- True cephalo-pelvic disproportion (where the fetal head is too large to pass through the maternal pelvis).
- Breech and face presentations, and most brow presentations.
- Note: Forceps can be used for the after coming head in complex breech deliveries.
- Preterm gestation (<34 weeks) for ventouse.
- High likelihood of any fetal coagulation disorder for ventouse.
Relative:
- Severe non-reassuring fetal status (‘acute fetal distress’), with station of the head above the level of the pelvic floor – i.e. fetal scalp not visible.
- Delivery of the second twin when the head has not quite engaged, or the cervix has reformed.
- Prolapse of the umbilical cord with fetal compromise when the cervix is completely dilated and the station is mid cavity.
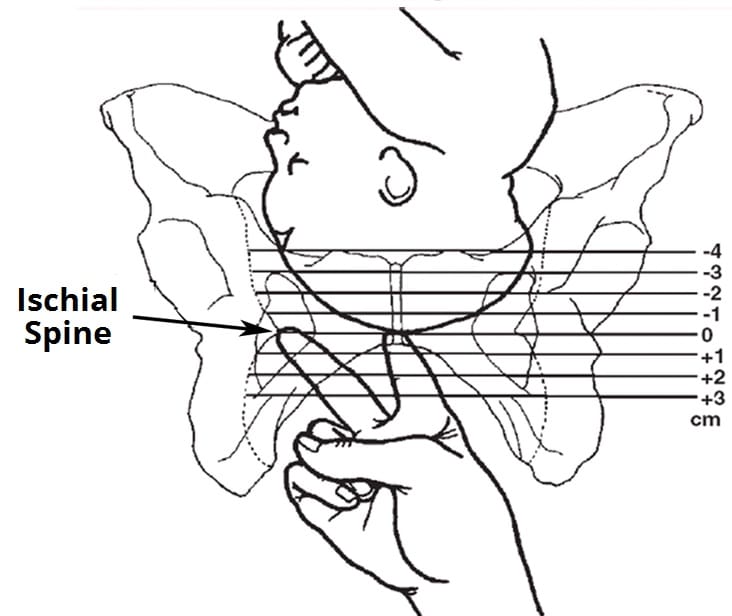
Fig 2 – Assessment of the fetal station is performed in relation to the ischial spines.
Pre-Requisites for Instrumental Delivery
In general, the pre-requisites for performing an instrumental delivery are:
- Fully dilated
- Ruptured membranes
- Cephalic presentation
- Defined fetal position
- Fetal head at least at the level of the ischial spines, and no more than 1/5 palpable per abdomen
- Empty bladder
- Adequate pain relief
- Adequate maternal pelvis
Classification
Operative vaginal deliveries are classified by the degree of fetal descent. The lower the classification, the less the risk of complications.
| Table 2 – Classification of Operative Vaginal Deliveries | ||
| Outlet | Low | Midline |
Any of the following:
|
Lowest presenting part (not caput) is +2, or further below the ischial spines.
Subdivided to
|
1/5 palpable abdominally
Lowest part is above +2, but is lower than the ischial spines Subdivided to
|
Complications
The complications of an operative vaginal delivery can be divided into fetal and maternal.
As a general rule, the lower the classification, the less rotation needed, and the fewer pulls – the lower the complication rate.
| Table 3 – Complications of an Instrumental Delivery | |
| Fetal | Maternal |
| Neonatal jaundice
Scalp lacerations Cephalhaematoma Subgaleal haematoma Facial bruising Facial nerve damage Skull fractures Retinal haemorrhage |
Vaginal tears
3rd/4th degree tears:
VTE Incontinence PPH Shoulder dystocia Infection |

