Hyperemesis gravidarum refers to persistent and severe vomiting during pregnancy, which leads to weight loss, dehydration and electrolyte imbalances.
It affects 0.3 – 3.6% of pregnant women, and is one of the more common reasons for hospital admission during pregnancy.
In this article, we shall look at risk factors, clinical features and management of hyperemesis gravidarum.
Aetiology and Pathophysiology
Nausea and vomiting of pregnancy (NVP) normally starts between 4 and 7 weeks’ gestation. It reaches a peak in the 9th week, and settles by week 20 in 90% of women.
Hyperemesis gravidarum (HG) is diagnosed when there is prolonged and severe NVP with:
- More than 5% pre-pregnancy weight loss
- Dehydration, and
- Electrolyte imbalances.
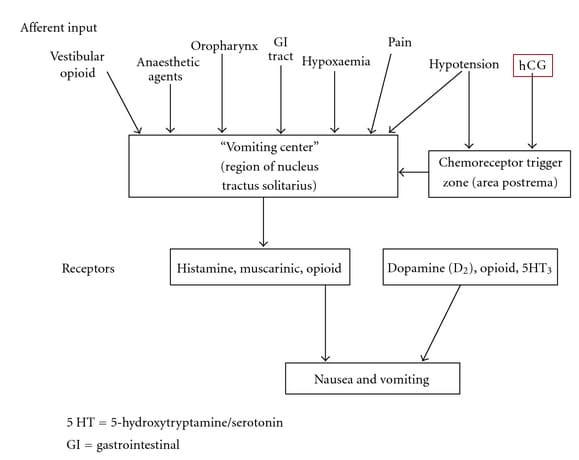
It is thought to be due rapidly increasing levels of beta human chorionic gonadotrophin (hCG) hormone, which is released by the placenta. High hCG stimulates the chemoreceptor trigger zone in the brainstem, which feeds into the vomiting centre of the brain.
Various other aetiological factors have also been proposed; including genetics, immunological and biosocial components.
Risk Factors
The risk factors for developing hyperemesis gravidarum include:
- First pregnancy
- Previous history of hyperemesis gravidarum
- Raised BMI
- Multiple pregnancy
- Hydatidiform mole
Clinical Features
The assessment of any nausea and vomiting in pregnancy should be made through history, examination and appropriate investigations.
An objective scoring system can be used to classify the severity, for example the Pregnancy-Unique Quantification of Emesis (PUQE) score; a score of 6 correlates to mild NVP, 7-12 moderate and 13-15 severe.
| History | Examination |
|
|
Differential Diagnosis
There are many possible causes for nausea and vomiting in pregnancy. An alternative diagnosis should particularly be considered if symptoms start after 10+6 weeks’ gestation:
- Gastroenteritis
- Cholecystitis
- Hepatitis
- Pancreatitis
- Chronic H. Pylori infection
- Peptic ulcers
- UTI or pyelonephritis
- Metabolic conditions
- Neurological conditions
- Drug-induced.
Investigations
The investigations in nausea and vomiting or hyperemesis gravidarum can be divided into bedside tests, laboratory tests and imaging.
Electrolyte levels are particularly important to monitor; as deranged levels are a hallmark of hyperemesis gravidarum.
Bedside Tests
- Weight
- Urine dipstick: quantify ketonuria (1+ ketones)
Laboratory Tests
- Mid-stream urine
- Full blood count: anaemia, infection, haematocrit (can be raised)
- Urea and Electrolytes: hypokalaemia, hyponatraemia, dehydration, renal disease
- Blood glucose: exclude diabetic ketoacidosis if diabetic
Refractory or Severe Cases
- Liver function tests: exclude liver disease e.g. hepatitis or gallstones, monitor malnutrition
- Amylase: exclude pancreatitis
- Thyroid function tests: hypo-/hyper-thyroid
- Arterial blood gas: exclude metabolic disturbances, monitor severity
Imaging
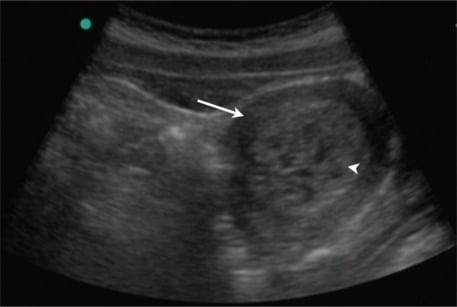
- Ultrasound scan: confirm viability, confirm gestation, exclude multiple pregnancy and trophoblastic disease.
Management
In the management of nausea and vomiting or hyperemesis gravidarum, the severity of symptoms determines the recommended management:
- Mild – should be managed in the community with oral antiemetics, oral hydration, dietary advice and reassurance.
- Moderate (or cases where community management has failed) – should be managed with ambulatory daycare. This involves IV fluids, parenteral antiemetics and thiamine. The patient should be managed until ketonuria resolves.
- Severe – inpatient management.
The recommended antiemetic therapies are shown in the box below. A combination of therapies should be used if there is no response to a single therapy.
IV rehydration should be with 0.9% saline. Potassium chloride should be added as guided by electrolyte monitoring.
Additional therapies include:
- H2 receptor antagonists or proton pump inhibitors: for reflux, oesophagitis or gastritis
- Thiamine: for prolonged vomiting to prevent Wernicke’s encephalopathy
- Thromboprophylaxis: for all women requiring admission
Recommended Antiemetic Therapies
First line:
- Cyclizine
- Prochlorperazine
- Promethazine
- Chlorpromazine
Second line:
- Metoclopramide (maximum 5 days due to risk of extrapyramidal side effects)
- Domperidone
- Ondansetron
Third line:
- Hydrocortisone IV
- Once symptoms improve, convert to prednisolone PO and gradually reduce dose until lowest maintenance dose is reached
Summary
- Hyperemesis gravidarum (HG) is diagnosed when there is prolonged and severe nausea and vomiting in pregnancy
- It is common, particularly in women with a history of HG
- HG is caused by rapidly increasing hCG
- The diagnosis is made via history, examination and investigation.
- The management of HG involves antiemetics and rehydration
- The severity of HG determines the most appropriate setting for management