Hormonal contraception uses the female steroid hormones oestrogen and progesterone and is a very effective method of preventing pregnancy, more so than barrier contraception. Hormonal contraception can be effectively split into two categories; ‘combined methods’ which contain both oestrogen and progesterone and ‘progesterone-only methods’ which contain only progesterone.
In this article we will cover the main methods of combined hormonal contraception, the mechanisms of action and the benefits and contraindications of such methods.
Mechanism of Action
Combined hormonal contraceptives act primarily to inhibit ovulation due to the negative feedback effect of the oestrogen and progesterone on the hypothalamo-pituitary axis. This prevents the surge in LH thus preventing ovulation. The progesterone also acts to inhibit proliferation of the endometrium, creating unfavourable conditions for implantation and increases the thickness of cervical mucus, preventing passage of sperm.
The period free of hormones, (pill-free break or taking placebos) causes a fall in hormonal concentration which leads to degeneration of the endometrium and menstrual bleeding.
Methods
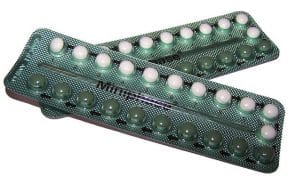
Fig 1. Combined oral contraceptive pill.
Combined Oral Contraceptive Pill
The COCP is commonly called ‘the pill’ and contains both oestrogen and progesterone. There are two types of combined oral contraceptive pills:
- Monophasic pills: every pill contains the same levels of oestrogen and progesterone.
- Phasic pills: the level of oestrogen and progesterone in the pills changes throughout the cycle.
There are also varying levels of oestrogen, with the pills classed as ‘low oestrogen pills’ containing only 20µg of ethinylestradiol.
Oral contraceptives come in packets of 21 or 28 tablets. Packets of 21 are taken consecutively for 21 days and then a 7 day break between packets where no pills are taken. The packets of 28 are taken consecutively for 28 days and there is no break before starting the next packet.
Monophasic pills:
This is the most common type of pill. Each pill contains the same amount of progesterone and oestrogen throughout the cycle. Examples include:
- Microgynon®30 – 30µg ethinylestradiol (oestrogen) and 150µg levonorgestrel (progesterone). Microgynon®30 is the most common monophasic pill used and is taken once daily for 21 days with a 7 day break between packs.
- Brevinor® – 35µg ethinylestradiol and 0.5mg norethisterone. Brevinor® is taken once daily for 21 days with a 7 day break between packs.
Phasic pills:
Phasic oral contraceptives contain a varying amount of oestrogen and progesterone across the cycle and can be biphasic, triphasic or quadraphasic depending on the number of different active tablets. It is very important for the patient to take the pills in the correct order due to the varying levels of hormones through the cycle. Examples include:
- Qlaira® – This is a quadraphasic combined oral contraceptive containing estradiol valerate and dienogest at varying levels through the cycle. Qlaira® is taken every day for 28 days without a break between packs, it contains 26 active pills and 2 inactive pills.
- BiNovum® – This is a biphasic pill containing 35µg of ethinylestradiol and varying levels of norethisterone. BiNovum® is taken for 21 days with a 7 day break between packets.

Fig 2. Contraceptive transdermal patch.
The Contraceptive Transdermal Patch
The contraceptive patch is a small 5cmx5cm patch that can be stuck onto the upper arm, abdomen, buttock or back to prevent pregnancy. The patch used in the UK is branded Ortho Evra® and it is a combined hormonal method which delivers 150µg norelgestromin and 25µg ethinyl estradiol per day. These hormones work in the same way as the COCP by preventing ovulation, thinning the endometrial lining and thickening cervical mucus.
The patch is applied and changed every 7 days over a period of 3 weeks (21 days in total) and then the patch is removed for 7 patch-free days where the individual will usually experience a withdrawal bleed.
The patch is extremely sticky and can be used whilst bathing and swimming.

Fig 3. Contraceptive vaginal ring
The Contraceptive Vaginal Ring
The vaginal ring (NuvaRing®) is a combined hormonal contraceptive method. The plastic ring is inserted into the vagina and delivers 120µg etonogestrel and 15µg ethinyl estradiol per day. These hormones work in the same way as the COCP by preventing ovulation, thinning the endometrial lining and thickening cervical mucus.
Once inserted the ring sits in the vagina for 21 days. It is then removed for 7 days before inserting the new ring.
Some women however may feel uncomfortable inserting or removing the ring.
Advantages
- Non invasive
- More effective than barrier methods if taken correctly
- Sex doesn’t need to be interrupted to use contraception
- Menses tends to become regular, lighter and less painful, also allowing for control over timing of menses
- Reduced risk of cancer of the ovary, uterus and colon
- Reduced risk of functional ovarian cysts
- Normal fertility returns immediately after stopping usage
Disadvantages
- User dependent
- Some temporary adverse effects such as headaches, breast tenderness and mood changes can be experienced by some women
- Blood pressure may increase
- Women may experience breakthrough bleeding and spotting for the first few months
- Increased risk of venous thromboembolism
- Small increase in risk of myocardial infarctions and strokes
- Small increase risk of breast and cervical cancer
Contraindications
- BMI greater than 35
- Breast feeding
- Smoking over the age of 35
- Hypertension
- History of or family history of venous thromboembolisms
- Prolonged immobility due to surgery or disability
- Diabetes mellitus with complications e.g. retinopathy
- History of migraines with aura
- Breast cancer or primary liver tumours
Effectiveness of Combined Hormonal Contraceptive Methods
Failure rates of combined hormonal contraceptive methods are lower than those for barrier contraception. Values are expressed as the percentage of women who will get pregnant in one year using the particular method.
| Perfect Use | Typical Rate | |
| Combined hormonal contraception | 0.3% | 9% |
Key Points to Consider
- Although hormonal contraception is extremely effective at preventing pregnancy it doesn’t protect against sexually transmitted infections so it’s important to counsel patients on safe sexual practices.
- With patient dependent hormonal contraception, it’s important to explain to the patient what to do if they miss a pill, the transdermal patch falls off/is wrongly removed or the vaginal ring becomes dislodged.
- Detailed information can be found in the Faculty of Sexual & Reproductive Healthcare (FSRH) UK Medical Eligibility Criteria (MEC) guidelines.
