Female genital mutilation (FGM) involves any procedure resulting in the partial or total removal of the external female genitalia, or other injury to the female genital organs for non-medical purposes. It is illegal to carry out FGM in the UK and it is internationally recognised as a human rights violation.
In this article we shall look at the epidemiology, types, complications and management of FGM. We will also discuss how to identify FGM in medical practice and outline the UK law and duties of healthcare professionals when managing FGM patients.
Side note: For the purposes of this article the term ‘female’ is used when referring to biological sex and not gender identity.
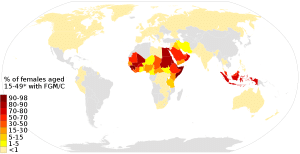
Epidemiology
It is estimated that 125 million women and girls globally have undergone FGM. It is a common occurrence in many African countries. Somalia, Guinea and Dijbouti have the highest prevalence with rates over 90%. Data demonstrates that it is also practiced in other countries, such as Iraq, Yemen, and Indonesia.
FGM in the UK
It is estimated that 137,000 women and girls in England and Wales, who were born in countries where the practice traditionally occurs, have undergone FGM. Over the three-month period of July to September 2022, 1650 women and girls had FGM identified when they attended NHS services.
Why is FGM performed?
FGM is practiced for a number of complex social, cultural and religious reasons, based on the mistaken belief that it will somehow provide benefit to the girl. For example, to preserve virginity, to uphold family honour or as a rite of passage. FGM is mainly performed on girls below the age of 15. Usually, it is carried out by traditional practitioners with no formal training. Worrying recent trends have shown that it is becoming increasingly common for FGM to be performed by medical professionals.
Classification of FGM:
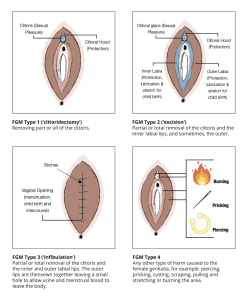
FGM has been classified into four types:
- Type 1 – The partial or total removal of the clitoris. This sometimes may involve the partial or total removal of the clitoral hood.
- Type 2 – The partial or total removal of the clitoris and the labia minora. This sometimes may also occur with removal of the labia majora.
- Type 3 – The making of a covering seal in order to narrow the vaginal opening. Also referred to as infibulation. This is done by cutting and altering the placement of the labia minora or majora, sometimes involving stitching. This may also be performed with the removal of the clitoris.
- Type 4 – This involves any and all other harmful procedures to the female genitalia for non-medical needs. This includes piercing, cutting, burning, scraping and pricking.
Complications of FGM
There are no health benefits to FGM and it results in many short- and long-term complications.
Short-term complications may include:
· Bleeding
· Urinary retention
· Genital swelling
· Severe pain
· Infection
· Poor wound healing
Long-term complications may include:
· Scarring
· Dyspareunia
· Urinary tract problems – eg infections, dysuria, urinary stricture or fistulae
· Impaired sexual function
· Dysmenorrhea
· Chronic infections – eg increased of risk Herpes Simplex type 2 and Bacterial vaginosis infections
· Psychological problems – eg PTSD, anxiety and depression
· Increased risk of obstetric complications – including prolonged and difficult labour, postpartum haemorrhage, needing neonatal resuscitation and stillbirth
Identifying FGM
It is important for all healthcare professionals to be aware of FGM and be able to recognise risk factors. This can help to identify cases, provide necessary medical care and potentially prevent future cases of FGM.
All patients should be screened for FGM at the time of booking their pregnancy, regardless of their country of origin, or ethnic background. Women with FGM have an increased risk of obstetric complications and so this will need to be managed appropriately. Additionally, obstetric consultations are an important opportunity for education, risk assessment and prevention of FGM to the unborn child and other female relatives.
Signs and scenarios in general practice or other clinical settings which may point to those with a higher risk of FGM include:
- The patient is known to have other family members that have undergone FGM
- The patient is part of a community known to practice FGM
- Women who refuse examination or cervical screening
- Discussion of extended visits with girls to countries where FGM is practised
- Girls presenting with repeated urinary, menstrual or abdominal problems
- Girls having difficulty sitting still for long periods
The Department of Health and Social Care have devised various templates to aid in the risk assessment of FGM in pregnant and non-pregnant women and girls, available here: https://www.gov.uk/government/publications/safeguarding-women-and-girls-at-risk-of-fgm.
When asking about FGM it is important to directly approach the subject in a mindful and non-judgemental manner. Remember that the patient may use different terminology, which may be appropriate for you to use depending on the circumstance – for example, cutting or female circumcision. If needed use translation services to aid the consultation, not family members. When able to do so, healthcare professionals should provide women with information about FGM, explain that it is illegal in the UK and that is has numerous serious health consequences.
UK law and mandatory reporting and recording
It is illegal to perform FGM in the UK. It is also a criminal offence to aid someone in carrying out FGM on themselves or others and to assist in the planning and procurement of FGM practices abroad.
Children:
- Reporting means making a referral to the police or social services. Healthcare professionals have a mandatory duty to report any confirmed cases of FGM to children under the age of 18. This should be done via the 101 non-emergency number within 1 month of the consultation. If a child is believed to be at risk of FGM then it is vital to seek guidance and report to social services and safeguarding.
Adults:
- There is a requirement to record data for all women identified as having FGM. This should be documented in their medical records.
- For non-pregnant women aged 18 and over, there is no duty to report unless a risk is posed to a related child.
- For pregnant women aged 18 and over, each case needs to be risk assessed individually. If the unborn child or any other related child are at risk of FGM then this must be reported to the police or social services. This then needs to be recorded in antenatal records, maternity documentation and the child’s personal health record.
Management of FGM
Women identified as having FGM can be offered:
- A referral to specialist gynaecology or FGM services
- A referral for psychological assessment and management
- Testing for HIV, hepatitis B and C as well as a sexual health screening.
Pregnant women with FGM should be managed as having a high obstetric risk and will most likely require consultant-led care unless there is a history of previous uncomplicated vaginal deliveries.
De-infibulation is a minor procedure that is performed for women with type 3 FGM. It involves incising along the scar tissue which is narrowing the vaginal opening and can be performed under local anaesthetic. This can allow for improved urinary and menstrual symptoms, comfortable sexual intercourse and child birth. In the obstetric setting, de-infibulation can be performed antenatally or intrapartum. Ideally it should be performed around 20 weeks gestation. Patients should be made aware that re-infibulation (re-closure of the vaginal opening) is illegal and will not be performed.
Key Learning Points:
- Any non-medical procedure that causes harm or injury to the female genitalia is categorised as FGM.
- FGM is illegal in the UK and is a human rights violation.
- There are four types of FGM which can cause serious lasting health issues.
- Professionals have a mandatory reporting duty for any cases of FGM to a minor under the age of 18.
- For pregnant and non-pregnant women over the age of 18, an individualised assessment needs to be conducted. This is done in order to evaluate the FGM risk posed to any related or unborn children before reporting.
- De-infibulation can be performed to widen the vaginal opening and improve symptoms of FGM complications. Re-infibulation is illegal.
If you or anyone you know has been affected by FGM please use the links below for further information, advice and support: https://www.nhs.uk/conditions/female-genital-mutilation-fgm/ https://www.rcog.org.uk/for-the-public/browse-all-patient-information-leaflets/female-genital-mutilation-fgm/
The NSPCC also has a helpline available to provide information and advice for professionals and people affected by FGM. Please use if you think a child’s wellbeing is at risk due to FGM – https://www.nspcc.org.uk/