A hysterectomy is the surgical removal of the uterus. It is a very common procedure, performed for a variety of indications.
In this article, we shall look at the classification, indications and complications of a hysterectomy.
Classification
A hysterectomy can be classified by the amount of tissue resected:
- Total hysterectomy – removal of the uterus and cervix.
- Sub-total hysterectomy – removal of the body of the uterus only, leaving the cervix behind.
- Total hysterectomy and bilateral salpingo-oophorectomy – removal of the uterus, cervix, fallopian tubes and ovaries.
- Radical hysterectomy – removal of the uterus and cervix, the parametrium, a vaginal cuff and part of or the whole of the fallopian tubes.
- This procedure is carried out in selected cases of cervical cancer.
- The ovaries may be removed or may be left behind, depending on the patient’s age.
Procedure
There are three main approaches to a hysterectomy. The principles and steps for each approach are the same (but in a different order).
- Abdominal – via an incision in the abdomen.
- Vaginal – via incision through the superior part of the vagina.
- Laparoscopic – via small incisions in the abdomen, and using laparoscopes and a uterine manipulator.
Mobilisation should be encouraged as soon as possible. Discharge is usually after 1-2 days for vaginal and laparoscopic hysterectomy, and 2-5 days for abdominal hysterectomy (depending on the type of incision – generally longer stay if midline incision).
Abdominal Hysterectomy
An abdominal hysterectomy may be performed through a low transverse incision, or through a midline incision. This depends on the indication and the size of the uterus – for example, a large fibroid uterus may necessitate a midline incision.
The steps for a simple total hysterectomy, after the abdomen is opened are as follows:
- The round ligaments are divided.
- If the tubes and ovaries are to be removed, the infundibulopelvic ligaments are ligated and tied (the ureters should be identified first).
- The uterovesical peritoneal fold is divided and the bladder reflected down past the cervix.
- The parametrial tissue is divided.
- The uterine vessels and ligated and tied.
- The paracervical tissue and uterosacral ligaments are ligated and tied.
- The vagina is opened and the uterus and cervix removed.
- The vagina is usually closed with an absorbable suture.
- Haemostasis is confirmed at all pedicles.
- The abdomen is closed.
Laparoscopic Hysterectomy
The above steps are identical for a total laparoscopic hysterectomy, except that the procedure is performed through several very small incisions, using a laparoscope and laparoscopic instruments. The specimen (uterus, cervix +/- tubes and ovaries) is removed through the vagina.
Bipolar energy may be used for coagulation of blood vessels with scissors for dissection, or more modern energy devices may be used. The vaginal vault may be closed laparoscopically or vaginally. It can also be performed using a robotic platform (available in some parts of the UK).
A general anaesthetic is required for abdominal and laparoscopic hysterectomy.

Fig 2 – A) Principles of a laparoscopic hysterectomy, B) Transvaginal extraction of the uterus in total laparoscopical hysterectomy.
Vaginal Hysterectomy
For a vaginal hysterectomy, no abdominal incisions are made and the procedure is performed entirely through the vagina.
The steps are as follows:
- Local anaesthesia is infiltrated around the cervix (front and back, not laterally).
- A circumferential incision is made around the cervix.
- The bladder is dissected off the cervix and reflected upwards.
- The anterior peritoneum is opened by cutting the utero-vesical peritoneal fold.
- The Pouch of Douglas is opened.
- The uterosacral ligaments are ligated and tied.
- The uterine arteries and ligated and tied.
- The round ligaments are ligated and tied.
- The tubes and ovaries may be taken in this pedicle, or may be preserved.
- The uterus and cervix are removed.
- The vagina is normally closed or the edges sutured to ensure haemostasis.
- The uterosacral ligaments may be fixed to the upper vagina to prevent prolapse of the vaginal vault.
Vaginal hysterectomy may be performed under regional anaesthesia (spinal/ epidural). A general anaesthetic is not required.
Indications
A hysterectomy has a number of possible indications. The following are the most common, but this is not an exhaustive list:
- Heavy menstrual bleeding
- Pelvic pain
- Uterine prolapse (vaginal hysterectomy)
- Gynaecological malignancy (usually ovarian, uterine or cervical)
- Risk reducing surgery, usually in cases of BRCA 1 or 2 mutations, or Lynch syndrome.
Hysterectomy may also be performed as a life saving procedure in the management of major postpartum haemorrhage.
Complications
There are some potential complications of a hysterectomy. As for any surgical procedure, the general complications include risk of haemorrhage, infection and pain. There is also a general anaesthetic risk.
The specific complications of hysterectomy include:
- Damage to the bladder and/or the ureter (seven women in every 1000) and/or long-term disturbance to the bladder function (uncommon)
- Damage to the bowel: four women in every 10 000 (rare)
- Haemorrhage requiring blood transfusion, 23 women in every 1 000 (common)
- Return to theatre because of bleeding/wound dehiscence, and so on: seven women in every 1000 (uncommon)
- Pelvic abscess/infection: two women in every 1000 (uncommon)
- Venous thrombosis or pulmonary embolism, four women in every 1000 (uncommon)
- Risk of death within 6 weeks, 32 women in every 100 000 (rare). The main causes of death are pulmonary embolism and cardiac disease.
If the ovaries are conserved, menopause may occur earlier (by 1-2 years) due to a change in the blood supply to the ovaries.
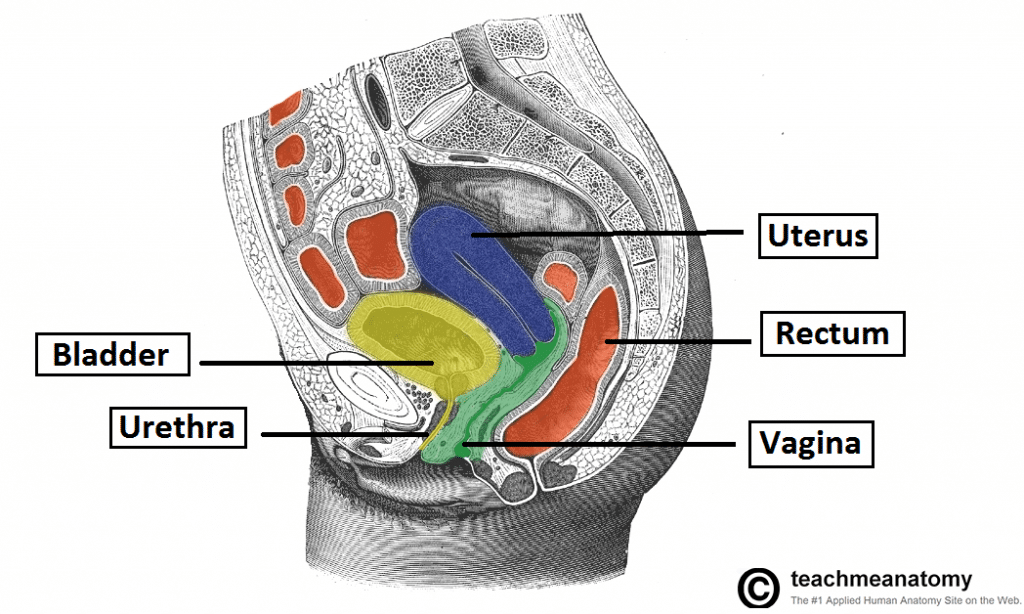
Fig 3 – Sagittal section of the female pelvis. Note the close anatomical relation of the bladder and bowel to the uterus – and damage to these structures is a complication of a hysterectomy.

