Uterine fibroids (leiomyomas) are benign smooth muscle tumours of the uterus.
They are the most common benign tumours in women, with an estimated incidence of 20-40%. The risk of a fibroid becoming malignant is 0.1%.
In this article, we shall look at the risk factors, clinical features and management of uterine fibroids.
Pathophysiology and Aetiology
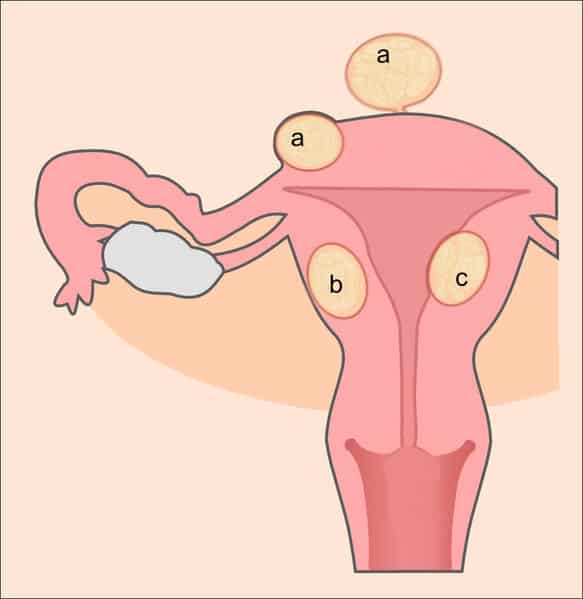
Fibroids (leiomyomata) are benign smooth muscle tumours arising from the myometrium of the uterus. They can be classified according to their position in the uterine wall:
- Intramural (most common) – confined to the myometrium of the uterus.
- Submucosal – develops immediately underneath the endometrium of the uterus, and protrudes into the uterine cavity.
- Subserosal – protrudes into and distort the serosal (outer) surface of the uterus. They may be pedunculated (on a stalk).
The pathogenesis of fibroids is poorly understood. Their growth is thought to be stimulated by oestrogen. Fibroids are usually benign and very rarely become malignant.
Risk Factors
The risk factors for developing fibroids include:
- Obesity
- Early menarche
- Increasing age
- Family history
- Women with a 1st degree relative affected carry a 2.5x increased risk.
- Ethnicity
- African-Americans are 3x more likely to develop fibroid than Caucasians.
Clinical Features
The majority of women with fibroids are asymptomatic – they are often discovered incidentally on pelvic or abdominal examination.
History
- Pressure symptoms +/- abdominal distention
- This includes urinary frequency or chronic retention.
- Heavy menstrual bleeding
- Subfertility – due to the obstructive effect of the fibroid.
- Acute pelvic pain (rare):
- May occur in pregnancy due to red degeneration. This is where the rapidly growing fibroid undergoes necrosis and haemorrhage.
- Rarely, pedunculated fibroids can undergo torsion.
Examination
A solid mass or enlarged uterus may be palpable on abdominal or bimanual examination. The uterus is usually non-tender.
Differential Diagnosis
The major differential diagnoses for uterine fibroids include:
- Endometrial polyp
- Ovarian tumours
- Leiomyosarcoma – malignancy of the myometrium.
- Adenomyosis – presence of functional endometrial tissue within the myometrium.
Investigations
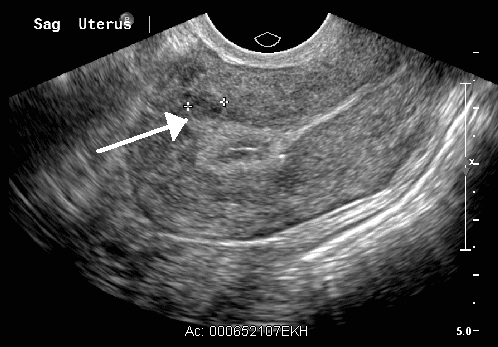
Imaging is the main investigation for suspected fibroids:
- Pelvic ultrasound
- MRI (rarely required, unless sarcoma is suspected)
Blood tests are usually reserved for patients where the diagnosis is unclear, or as a pre-operative work-up if surgery is indicated.
Management
There are both medical and surgical options for the management of uterine fibroids. Asymptomatic patients with small fibroids often do not need treatment.
Medical
- Tranexamic or mefanamic acid
- Hormonal contraceptives
- Useful to control menorrhagia
- Includes the COCP, POP and Mirena IUS.
- GnRH analogues (Zolidex)
- Suppresses ovulation, inducing a temporary menopausal state.
- Useful pre-operatively to reduce fibroid size and lower complications.
- Can be used for 6 months only, due to the risk of osteoporosis
- Selective Progesterone Receptor Modulators (Ulipristal / Esmya)
- Reduces size of fibroid and menorrhagia
- Useful pre-operatively or as an alternative to surgery
- Use of Ulipristal is restricted due to risk of severe liver injury
Surgical
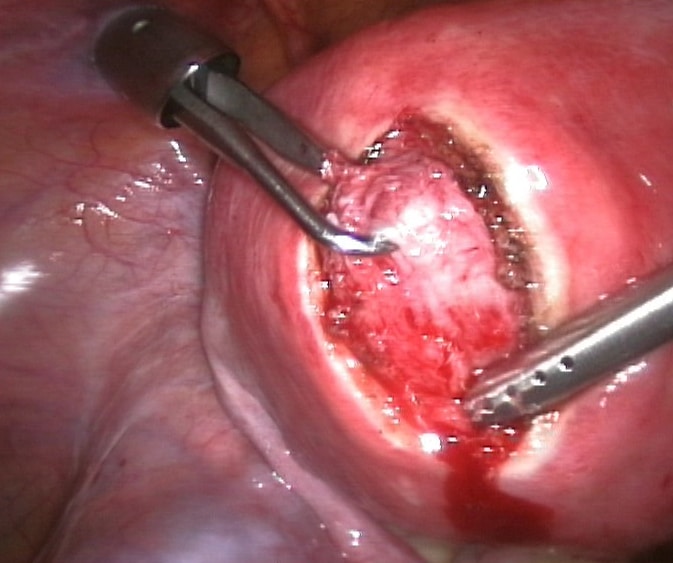
- Hysteroscopy and Transcervical Resection of Fibroid (TCRF)
- Useful for submucosal fibroids
- Myomectomy
- Option in women wanting to preserve their uterus
- Uterine Artery Embolization (UAE)
- Performed by a radiologist via the femoral artery
- Commonly causes pain and fever post-operatively
- Hysterectomy
Complications:
- Iron deficiency anaemia
- Compression of pelvic organs
- Recurrent urinary tract infections
- Incontinence
- Hydronephrosis
- Urinary retention
- Subfertility/infertility
- Degeneration
- Torsion