Induction of labour (IOL) is the process of starting labour artificially. Whilst most women will go into labour spontaneously by week 42 of gestation, roughly 1 in 5 pregnancies will require an induction.
As a general rule, IOL is performed when it thought that the baby will be safer delivered than remaining in utero. Alternatively, it may be for reasons concerning the mother’s health.
In this article we will discuss the indications, contraindications, methods, monitoring and risks of the induction of labour.
Indications
Induction of labour is indicated when it is thought that delivering the baby will be safer for the baby and/or the mother, than for the baby to remain in utero.
Note: In the UK, NICE guidelines (2008) state that induction of labour should NOT be offered on maternal request alone.
Prolonged Gestation
Women with uncomplicated pregnancies should be offered IOL between 40+0 to 40+14 weeks’ gestation. The aim is to avoid the risks of fetal compromise and stillbirth associated with prolonged gestation (thought to be secondary to placental ageing).
If the patient declines an induction of labour, the frequency of monitoring from 42 weeks onwards should be increased.
Premature Rupture of Membranes
For premature rupture of membranes (>37 weeks’ gestation) offer IOL, or alternatively offer expectant management for a maximum of 24 hours (any longer increases the risk of ascending infection – chorioamnionitis). 84% of women will spontaneously go into labour within the first 24 hours.
For preterm premature rupture of membranes (PPROM):
- <34 weeks’ gestation – delay IOL unless obstetric factors indicate otherwise e.g. fetal distress.
- >34 weeks’ gestation – the timing of IOL depends on risks vs benefits of delaying pregnancy further e.g. increased risk of infection.
Maternal Health Problems
Common examples of maternal health problems include hypertension, pre-eclampsia, diabetes and obstetric cholestasis.
The decision to induce will depend on the health of the mother and the fetus.
Fetal Growth Restriction
Fetal growth restriction is the second most common indication for induction of labour. The aim is to deliver the baby prior to fetal compromise.
Intrauterine Fetal Death
In cases of intrauterine fetal death, induction of labour should be offered if mother is physically well with intact membranes.
Contraindications
The contraindications for induction of labour are generally the same as for vaginal delivery. They can be divided into absolute contraindications and relative contraindications (Table 1).
| Table 1 – Contraindications for Induction of Labour | |
| Absolute Contraindications | Relative Contraindications |
| Cephalopelvic disproportion
Major placenta praevia Vasa praevia Cord prolapse Transverse lie Active primary genital herpes Previous classical Caesarean section |
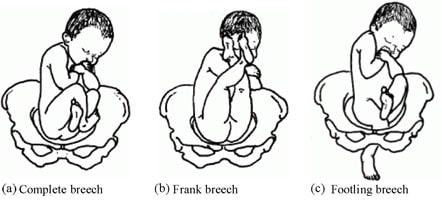
Breech presentation
Triplet or higher order pregnancy Two or more previous low transverse caesarean sections
|
If a woman has had a previous caesarean section, IOL can be offered safely after she has been seen and assessed by a consultant (who is happy for IOL to proceed). However, the mother should be made aware of an increased risk of emergency caesarean and uterine rupture.
Methods of Induction
There are three main methods of induction – vaginal prostaglandins, amniotomy and membrane sweep. There is a lack of evidence regarding other methods of IOL, including homeopathy, acupuncture and sexual intercourse.
Vaginal Prostaglandins
Vaginal prostaglandins form the mainstay of induction of labour, and are the preferred primary method as advised by NICE guidelines (2008).
Prostaglandins act to prepare the cervix for labour by ripening it, and also have a role in the contraction of the smooth muscle of the uterus. They come as either a tablet, gel or a controlled-release pessary:
- Tablet/gel regimen: 1 cycle = 1st dose, plus a 2nd dose if labour has not started 6 hours later.
- Pessary regimen: 1 cycle = 1 dose over 24 hours.
There is a recommended maximum of one cycle in 24 hours (IOL can sometimes take multiple days).
Amniotomy
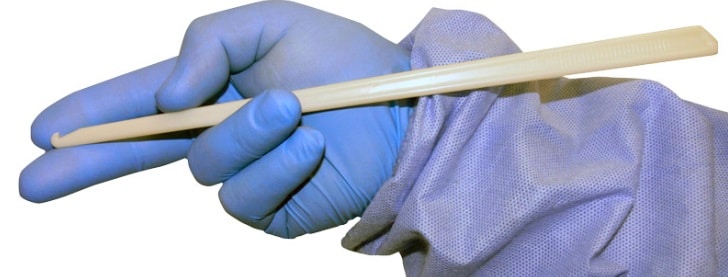
An amniotomy is where the membranes are ruptured artificially using an instrument called an amnihook. As with a membrane sweep, this process releases prostaglandins in an attempt to expedite labour. It is only performed when the cervix has been deemed as ‘ripe’ (see Bishop Score below).
Often, an infusion of artificial oxytocin (Syntocinon) will be given alongside an amniotomy, acting to increase the strength and frequency of contractions. The aim is to start low and titrate upwards until there are 4 contractions every 10 minutes.
NICE guidelines (2008) advise that amniotomy +/- oxytocin should NOT be used as the primary method of IOL, unless use of prostaglandins are contraindicated e.g. high risk of uterine hyperstimulation.
Membrane Sweep
The membrane sweep is offered at 40 and 41 weeks’ gestation to nulliparous women, and 41 weeks to multiparous women.
It is classified as an adjunct of IOL. Performing it increases the likelihood of spontaneous delivery, reducing the need for a formal induction.
The procedure is performed by inserting a gloved finger through cervix and rotating it against the fetal membranes, aiming to separate the chorionic membrane from the decidua. The separation helps to release natural prostaglandins in an attempt to kick-start labour.
Monitoring
Bishop Score
The bishop score is an assessment of ‘cervical ripeness‘ based on measurements taken during vaginal examination. It is checked prior to induction, and during induction to assess progress (6 hours post-table/gel, 24 hours post-pessary):
- Score of ≥ 7 – suggests the cervix is ripe or ‘favourable’ – this means that there is a high chance of a response to interventions made to induce labour (i.e. induction of labour is possible).
- Score of <4 – suggests that labour is unlikely to progress naturally and prostaglandin tablet/gel/pessary will be required
Failure of a cervix to ripen despite use of prostaglandins may result in the need for a caesarean section.
| Table 2 – Modified Bishop Score (RCOG 2001) | ||||
| Cervical Feature | 0 | 1 | 2 | 3 |
| Dilation (cm) | <1 | 1-2 | 2-4 | >4 |
| Length (cm) | >4 | 2-4 | 1-2 | <1 |
| Station (relative to ischial spines) | -3 | -2 | -1/0 | +1/+2 |
| Consistency | Firm | Average | Soft | – |
| Position | Posterior | Mid/anterior | – | – |
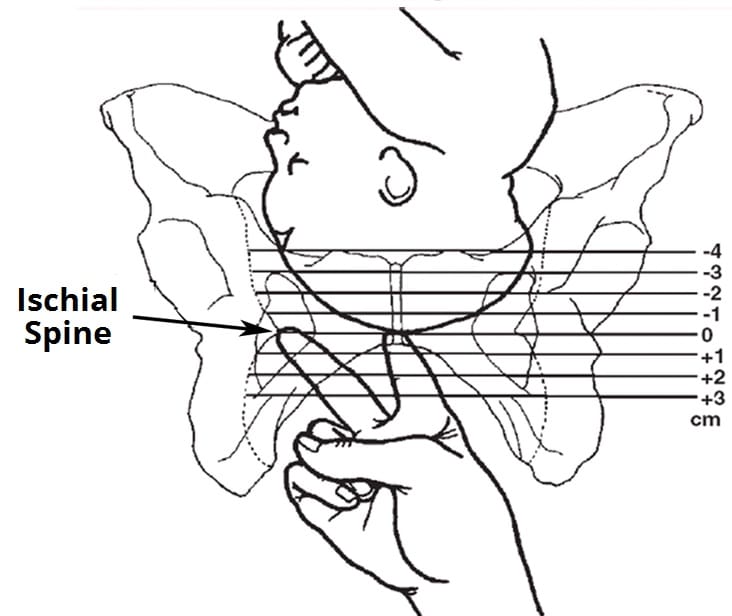
Fig 3 – Measuring the station of the fetus, in relation to the ischial spines.
Cardiotocography (CTG)
Prior to induction of labour, a reassuring fetal heart rate must be confirmed by cardiotocography.
After initiation of IOL, when contractions begin assess fetal heart rate using continuous CTG until a normal rate is confirmed. Subsequently assess using intermittent auscultation.
If an oxytocin infusion is started, monitor using continuous CTG throughout labour.
Complications
The complications of induction of labour are:
- Failure of induction (15%) – offer a further cycle of prostaglandins, or a caesarean section.
- Uterine hyperstimulation (1-5%) – contractions last too long or are too frequent, leading to fetal distress. Can be managed with tocolytic agents (anti-contraction) such as terbutaline.
- Cord prolapse – can occur at time of amniotomy, particularly if the presentation of the fetal head is high.
- Infection – risk is reduced by using pessary vs tablet/gel, as fewer vaginal examinations are required to check progress.
- Pain – IOL is often more painful than spontaneous labour. Often epidural analgesia is required.
- Increased rate of further intervention vs spontaneous labour – 22% require emergency caesarean sections, and 15% require instrumental deliveries.
- Uterine rupture (rare)