A speculum is a device used to look inside in the vagina and observe the cervix. A speculum examination is often performed alongside a bimanual examination, as part of a complete gynaecological workup.
In this article, we shall look at how to perform an speculum examination in an OSCE-style setting.
Introduction
- Introduce yourself to the patient
- Wash your hands
- Explain to the patient what the examination involves and why it is necessary
- For example: “I will be passing a speculum, which is a plastic/metal instrument, through the vagina to visualise the neck of the womb.”
- Reassure them that this should not be painful, but you will stop immediately if it becomes too uncomfortable
- Obtain verbal consent
- Request a chaperone
Preparation
- The patient ought to have an empty bladder, as this can make the examination less uncomfortable
- Ask the patient to remove all clothing from the waist down and any sanitary protection
- Cover with sheet when appropriate
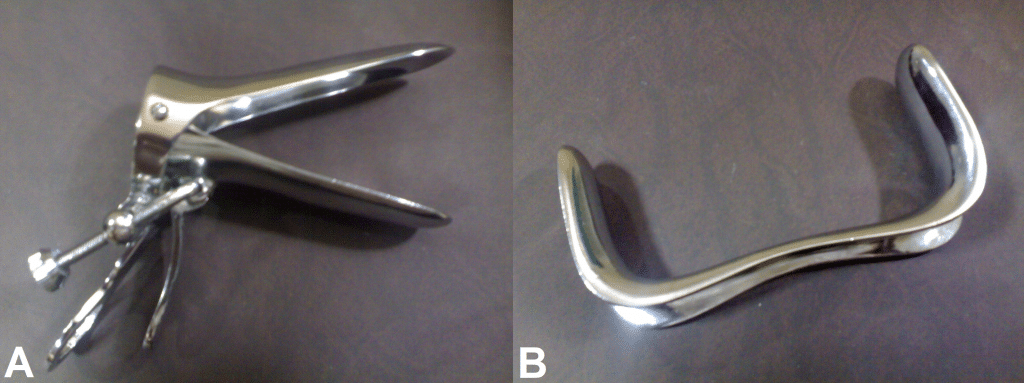
- Prepare your equipment: gloves, lubricant, speculum (for example Cusco’s speculum) +/- smear, swabs, Pipelle biopsy.
Abdominal Examination
- Inspect the abdomen for scars and ascites
- Palpate the abdomen for masses and tenderness
- Palpate the groin for inguinal lymphadenopathy
External Examination
The patient should be laid on their back, with legs bent at the hip (feet towards their buttocks), and asked to flop their knees apart.
- Put on a pair of gloves
- Inspect the external genitalia for:
- Deficiency associated with childbirth
- Abnormal secondary sexual characteristics – hair distribution, cliteromegaly
- Skin abnormalities – lesions, warts, erythema
- Discharge – colour, consistency
- Bleeding
- Swellings of the vulva – tumours, cysts (sebaceous, Bartholin’s)
- Ask the patient to cough or strain to observe any incontinence or prolapse
- Palpate the labia majora with the index finger and thumb for any swellings
Speculum Examination
- Lubricate the speculum and warn the patient
- Part the labia using your left hand
- Gently insert the speculum with your right hand:
- Fully insert the speculum with the screw facing sideways and the blades vertical
- Rotate 90 degrees during insertion so the screw faces upwards and the blades become horizontal
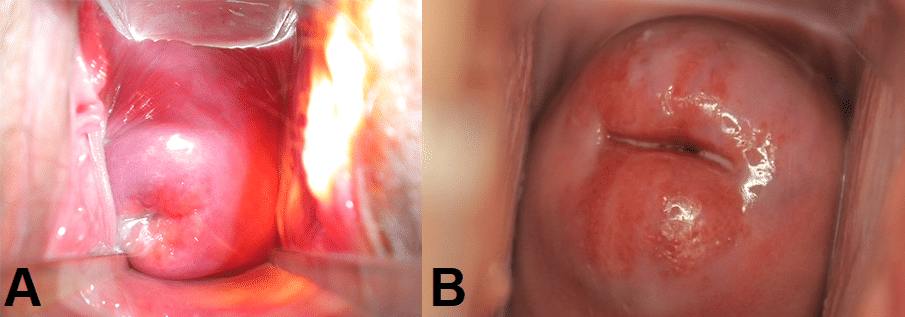
- Slowly open the blades and use light to inspect the cervix
- Tighten the screw to hold open the speculum so you can use your right hand for swabs or Pipelle biopsy if necessary
- Look for:
- Abnormal discharge
- Erosions
- Ulcerations
- Growths
- Inflammation
- Bleeding
- Polyps
- Ectropion
- At this point swabs/endometrial biopsy should be taken if required
- To remove the speculum, undo the screw to allow the blades to close (leave open slightly to not pinch the vaginal walls), rotating back 90 degrees and gently remove
To Complete the Examination
- Thank the patient and allow them to get dressed in private
- Dispose of your gloves and wash your hands
- Once the patient is dressed you can summarise the findings and suggest further investigations
- Send any specimens with a request form
Special Circumstances
Sim’s Speculum
A Sim’s speculum can be used to assess prolapse:
- Ask the patient to lie on her left side and bring her knees to her chest
- Insert the blade of the speculum along the posterior wall of the vagina to hold it back
- Ask the woman to cough whilst looking for uterine descent and cystocoele
- Repeat whilst holding back the anterior wall, looking for rectocoele/enterocoele
Obtaining Swabs
Swabs often required in cases of suspected infection:
- Pick up the sample tube with the right hand and place it in the left hand (with the speculum secured with the screw) and remove the lid if a separate one is present. Sometimes using the chaperone is useful.
- Take out the swab with the right hand and perform swabs in this order
- Hi-vaginal charcoal media swab – circle around the high vaginal wall once (BV, TV, Candida, group B strep)
- Endocervical charcoal media swab – place in endocervical canal and do a 360-degree sweep (gonorrhoea)
- Endocervical chlamydia swab – scrub endocervical region for 10-30 seconds
- Place the used swab back into the tube in your left hand, close the lid and label the specimens
Endocervical Smear
The cervical smear is used to detect precancerous changes in the cervix:
- Pass the cytobrush through the vagina (which is held open by the speculum), into the endocervical canal
- Turn the brush 360 degrees 5 times
- Introduce the brush to the specimen pot and move the brush against the bottom of the pot to dislodge cells into the liquid
- Label the specimen and send it off for liquid based cytology