Amenorrhoea and oligomenorrhoea are symptoms related to the frequency of menstrual periods.
In this article, we shall look at the causes of amenorrhoea and oligomenorrhoea, investigations that can be performed, and management of the common conditions.
Classification
Amenorrhoea refers to the absence of menstrual periods. It is subcategorised into primary and secondary causes.
- Primary – failure to commence menses (absence of menarche):
- Girls aged 16+, in the presence of secondary sexual characteristics such as pubic hair growth and breast development
- Girls aged 14+, in the absence of secondary sexual characteristics
- Secondary – cessation of periods for more than six months after the menarche (after excluding pregnancy).
Oligomenorrhea refers to irregular periods with intervals between menstrual cycles of more than 35 days and/or less than nine periods per year.
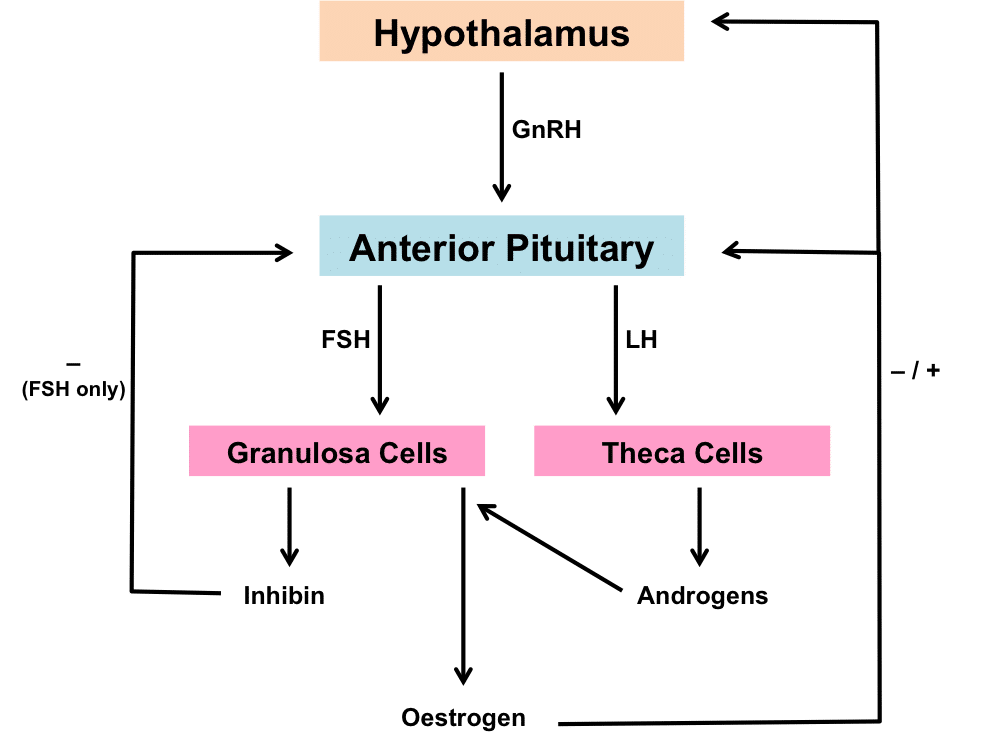
Pathophysiology
To achieve regular menstrual cycles, all components of the hypothalamic-pituitary-ovarian axis needs to be functioning appropriately.
Learn more about the HPG axis here.
Aetiology – Amenorrhoea
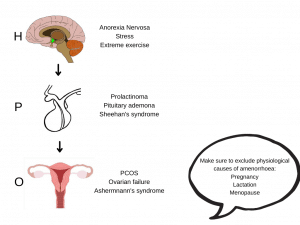
Hypothalamic Causes
Disease of the hypothalamus can reduce the secretion of GnRH. This, in turn, decreases the pulsatile release of LH and FSH from the anterior pituitary gland – causing anovulation.
Causes of hypothalamic amenorrhoea include:
- Functional disorders (e.g. eating disorders, exercise) – high level exercise or eating disorders suppress GnRH production and subsequently lead to low oestradiol levels, via ghrelin and leptin.
- Severe chronic conditions – such as psychiatric disorders, thyroid disease and sarcoidosis.
- Kallmann syndrome – an X-linked recessive disorder characterised by failure of migration of GnRH cells.
Pituitary Causes
The anterior pituitary gland releases LH and FSH, which are necessary for menses to occur. Common causes of pituitary amenorrhoea include:
- Prolactinomas – Represent 40-50% of all pituitary tumours. They secrete high levels of prolactin, which suppresses GnRH secretion. This causes anovulation, amenorrhoea and galactorrhoea.
- Other pituitary tumours (e.g. Acromegaly or Cushing’s syndrome) – gonadotrophin deficiency from mass effect of the tumour (+/- hyperprolactinaemia) induces menstrual irregularities.
- Sheehan’s syndrome – post-partum pituitary necrosis secondary to massive obstetric haemorrhage. Patients can have varying degree of anterior pituitary hormone deficiency.
- Destruction of pituitary gland – such as radiation or autoimmune disease.
- Post-contraception amenorrhoea – Prolonged use of contraceptives can cause long-term downregulation of the pituitary gland and irregular/absent periods or lack of ovulation which persists.
- This is most commonly seen with Depo-Provera, where it can take up to 18 months for menses to resume.
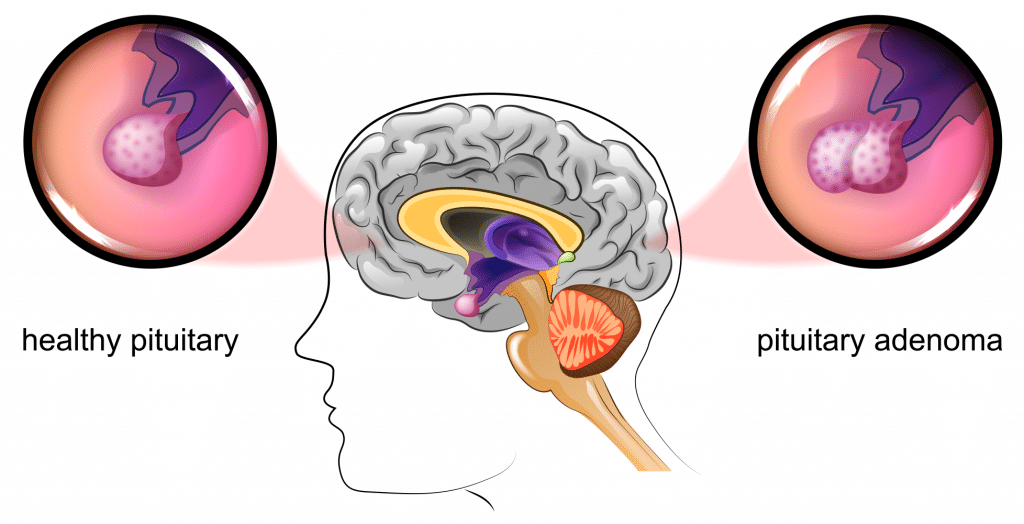
Fig 2 – Pituitary adenomas are a common cause of pituitary amenorrhoea.
Ovarian Causes
- Polycystic ovarian syndrome (PCOS) – more commonly causes oligomenorrhoea, but can present with amenorrhoea. It causes high androgen levels, leading to hirsutism, acne and weight gain.
- Turners syndrome (45 X0) – a genetic condition that causes amenorrhoea, failure to develop secondary sexual characteristics and almost universal infertility. Patients display a range of other features associated with the condition including a short stature, webbed neck and aortic coarctation.
- Premature ovarian failure – This is defined as primary ovarian insufficiency before the age of 40 associated with menopausal symptoms such as hot sweats or night sweats. Hormone profile tests show low oestrogen levels with high FSH.
Adrenal Gland
Disease of the adrenal gland can affect ovulation. Late onset/mild congenital adrenal hyperplasia is an autosomal recessive inherited condition which is caused by partial deficiency of 21 hydroxylase (an enzyme required for synthesis of cortisol and aldosterone).
Women present with early development of pubic hair, irregular or absent periods, hirsutism and acne. High levels of 17- hydroxyprogesterone are present in the blood.
Genital Tract Abnormalities
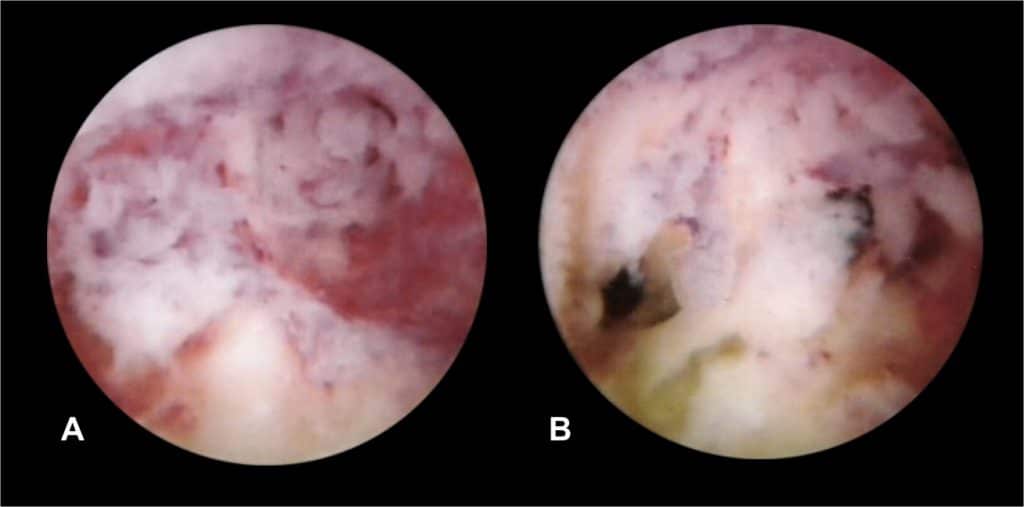
Any obstruction to the normal menses flow causes concealed bleeding and pain.
- Ashermann’s syndrome – can occur secondary to instrumentation of the uterus typically following SMM (surgical management of miscarriage). This damages the basal layer of the endometrium which causes intrauterine adhesions which fail to respond to oestrogen stimulus.
- Imperforate hymen/Transverse vaginal septum – a mechanical obstruction.
- Mayer-Rokitansky-Kuster-Hauser syndrome – characterised by agenesis of the Mullerian-duct system in varying degrees. This translates to congenital absence of the uterus and upper two thirds of the vagina and therefore a cause of primary amenorrhoea.
Causes of Amenorrhoea
Aetiology – Oligomenorrhoea
There is considerable overlap between oligomenorrhoea and secondary amenorrhoea.
Common causes include:
- PCOS
- Contraceptive/Hormonal treatments
- Perimenopause
- Thyroid disease/Diabetes
- Eating disorders/excessive exercise
- Medications e.g. anti-psychotics, anti-epileptics
Investigations and Diagnosis
Firstly, the menstrual irregularity must be classified into oligomenorrhoea, primary or secondary amenorrhoea as per the definitions above.
A focused and detailed history covering details of the periods, including what age the periods began, cycle length, development of secondary sexual characteristics, associated symptoms and past medical/surgical history will help to identify the cause.
A step-wise approach is necessary to identify the abnormality:
- Pregnancy test
- Blood tests:
- Thyroid function tests (TFTS) and prolactin.
- FSH/LH/Oestradiol/Progesterone/Testosterone.
- 17 hydroxyprogesterone (congenital adrenal hyperplasia)
- Karyotyping – if suspecting a genetic abnormality
- Ultrasound scan – to visualise ovaries and pelvic anatomy
- Progesterone challenge test to elicit a withdrawal bleed:
- A bleed suggests there are adequate levels of oestrogen however the patient is not ovulating i.e. PCOS.
- No bleed could mean there are very low levels of oestrogen or an outflow obstruction.
| GnRH | FSH | LH | LH:FSH ratio | Oestrogen | Testosterone | Prolactin | |
| Hypothalamic | ↓ | ↔ | ↓↔ | ↓ | ↓ | ||
| Prolactinoma | ↓ | ↑ | |||||
| PCOS | ↔ | ↑ | ↑ | ↔↑ | |||
| Premature ovarian failure | ↑ | ↑ | ↓ |
Management
Treatment will depend upon the exact cause of the oligomenorrhoea/amenorrhoea. However the general aims include:
Regulating Periods
The contraceptive pill in the form of either the combined (COCP) or the progesterone-only pill can help to regulate the periods and keeps the lining of the womb thin thereby reducing the long term risk of endometrial cancer.
The intrauterine system (IUS) can be useful in stopping or significantly reducing duration and flow of menses in women suffering from heavy, irregular periods.
Hormone Replacement
Women with premature ovarian failure/insufficiency should receive cyclical hormone replacement therapy with oestrogen (and progesterone if they have a uterus). This treats the symptoms of menopause, decreases the risk of cardiovascular disease and maintains bone density to prevent osteoporosis.
Calcium and Vitamin D supplementation is also recommended often following a bone density scan.
Symptom Control
A number of medications can be used to manage excessive hair growth including particular types of the COCP eg Yasmin, cyproterone actetate, spironolactone and finasteride.
Acne treatments include antibiotics and topical treatments such as benzoyl peroxide and topical retinoids. Patients with severe acne could be referred to a dermatologist for consideration of Isotretinoin (Roaccutane).
Lifestyle Advice
Hypothalamic amenorrhoea secondary to eating disorders or excessive exercise require a strict regime to increase body fat and stimulate GnRH production which should help to re-introduce the menstrual cycles.
Women with polycystic ovarian syndrome however need support with a healthy living schedule consisting of a balanced diet and regular exericise. Some patients would be suitable for weight loss medication such as orlistat, and statins if they have high cholesterol.
Treating Underlying Disorder
Both hyperthyroidism and hypothyroidism can result in menstrual disturbances:
- Hypothyroidism – the decreased T3/T4 causes upregulation of TRH which stimulates the secretion of prolactin therefore LH/FSH is inhibited.
- Hyperthyroidism – increased sex hormone binding globulin (SHBG) secretion secondary to high T3/T4 reduces the ratio of free/bound estradiol required to trigger the LH spike necessary for ovulation.
Assessment of thyroid function with a blood test and appropriate treatment with levothyroxine, carbimazole or propylthiouracil is necessary. Radioactive iodine may be suitable in selected cases.
Improving Fertility
Clomifene is used to stimulate ovulation as a means to treat infertility. Metformin can be used in polycystic ovarian syndrome to induce ovulation, as well as treating the insulin resistance commonly associated with this condition. It also has a role in regulating periods and reduces circulating androgen levels.
In Vitro Fertilisation (IVF) would be available to women as a last resort.
Surgery
Surgical intervention is the primary treatment for pituitary tumours and genital tract abnormalities. Pituitary adenomas are most commonly removed by a trans-sphenoidal approach.