Primary post-partum haemorrhage is the loss of >500 ml of blood per-vagina within 24 hours of delivery. It can be classified into two main types:
- Minor PPH – 500-1000ml of blood loss
- Major PPH – >1000ml of blood loss
It is a major cause of obstetric morbidity and mortality worldwide.
In this article, we shall examine the risk factors, clinical features and management of a primary post-partum haemorrhage.
Aetiology and Risk Factors:
The causes for primary post-partum haemorrhage can be broadly categorised by the 4 T’s – tone, tissue, trauma and thrombin.
Tone
‘Tone’ refers to uterine atony, which is the most common cause of primary post-partum haemorrhage. This is where the uterus fails to contract adequately following delivery, due to a lack of tone in the uterine muscle.
The risk factors for uterine atony include:
- Maternal profile: Age >40, BMI > 35, Asian ethnicity.
- Uterine over-distension – multiple pregnancy, polyhydramnios, fetal macrosomia.
- Labour – induction, prolonged (>12 hours).
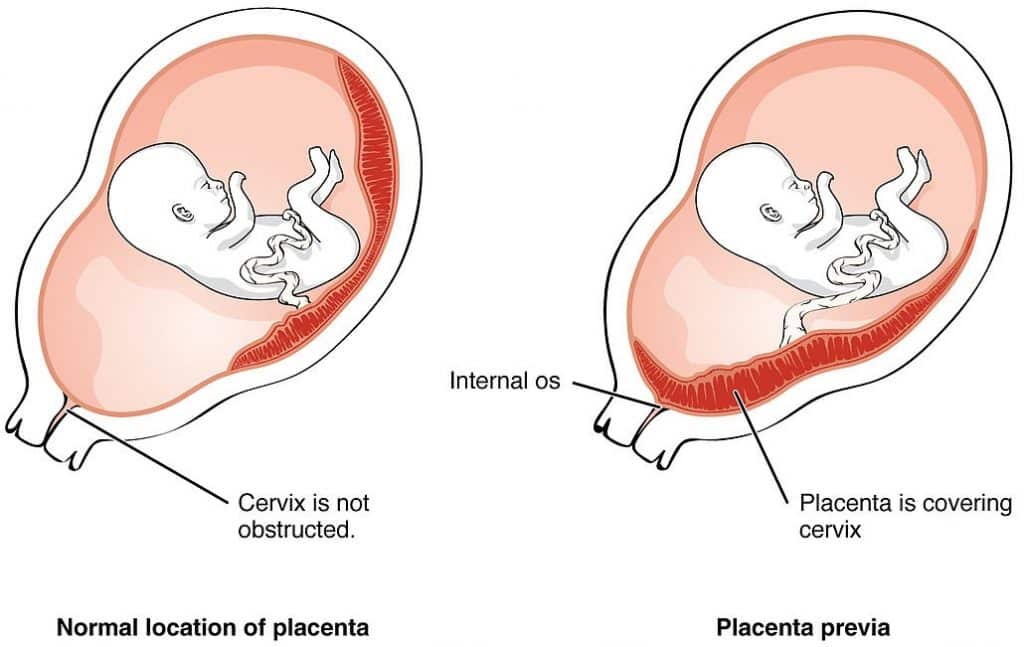
- Placental problems – placenta praevia, placental abruption, previous PPH.
Tissue
‘Tissue’ refers to retention of placental tissue – which prevents the uterus from contracting. It is the second most common cause of 1° PPH
Trauma
This refers to damage sustained to the reproductive tract during delivery (e.g. vaginal tears, cervical tears). Risk factors include:
- Instrumental vaginal deliveries (forceps or ventouse)
- Episiotomy
- C-section
Thrombin
‘Thrombin’ refers to coagulopathies and vascular abnormalities which increase the risk of primary post-partum haemorrhage:
- Vascular – Placental abruption, hypertension, pre-eclampsia.
- Coagulopathies – von Willebrand’s disease, haemophilia A/B, ITP or acquired coagulopathy i.e. DIC, HELLP.
Clinical Features
The main feature of a post-partum haemorrhage is bleeding from the vagina.
If there is substantial blood loss, the patient may complain of dizziness, palpitations, and shortness of breath.
On Examination:
- General examination may reveal haemodynamic instability with tachypnoea, prolonged capillary refill time, tachycardia, and hypotension.
- Abdominal examination may show signs of uterine rupture i.e. palpation of fetal parts as it moves into the abdomen from the uterus.
- Speculum examination may reveal sites of local trauma causing bleeding.
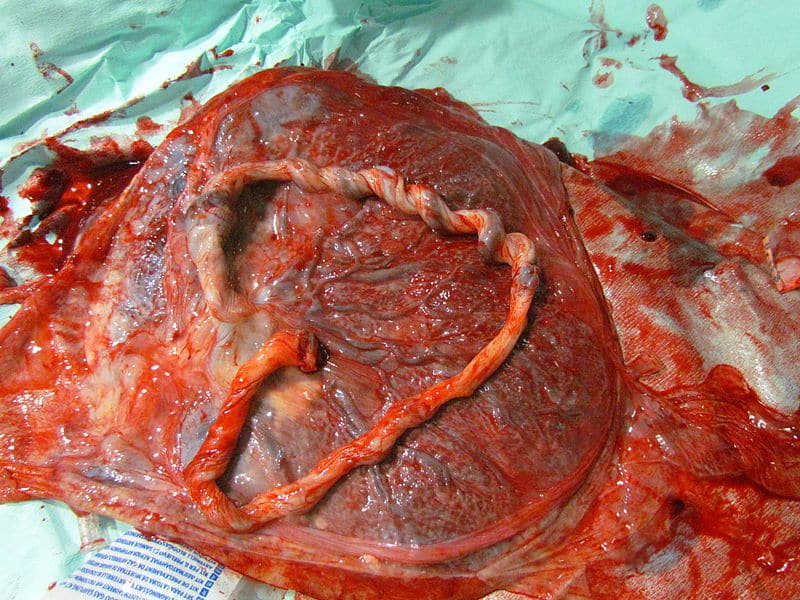
- Examine the placenta to ensure that the placenta is complete (a missing cotyledon or ragged membranes could both cause a PPH).
Investigations
The initial laboratory tests in primary post-partum haemorrhage include:
- Full blood count
- Cross match 4-6 units of blood
- Coagulation profile
- Urea and Electrolytes
- Liver function tests
Management
The management of primary post-partum haemorrhage should include the simultaneous delivery of TRIM:
- Teamwork (Immediate Management)
- Resuscitation (Immediate Management)
- Investigations and Monitoring (Immediate Management)
- Measures to arrest bleeding (Definitive Management)
Immediate Management
- Teamwork – Involve appropriate colleagues for minor and major PPH, including the midwife in charge and midwives, obstetricians, anaesthetists, blood bank, clinical haematologist and porters. Communication between the team, and diligent documentation is vital.
- Investigations and Monitoring – Investigations as above. Monitoring should include RR, O2 sats, HR, BP, temperature every 15 mins. Consider catheterisation and insertion of a central venous line.
Resuscitation
Resuscitate the patient via an A-E approach:
- Airway
- Protect airway (may lose it with reduced levels of consciousness).
- Breathing
- 15L of 100% oxygen through non-rebreathe mask.
- Circulation:
- Assess circulatory compromise (Cap refill, HR, BP, ECG)
- Insert two large bore (14G) cannulas and take blood samples (see below)
- Start circulatory resuscitation. Give cross-matched blood as soon as it is available, until then give up to 2L of warmed crystalloid and 1-2L of warmed colloids, then transfuse O negative or uncross matched group specific blood.
- Additional blood productions i.e. factor VIIa in Haemophilia A, and if major haemorrhage protocol activated may need to supplement fresh frozen plasma, platelets, fibrinogen. (Discussion with blood bank)
- Disability
- Monitor patient’s Glasgow coma score (GCS).
- Exposure
- Expose patient to identify bleeding sources.
Definitive Management
The definitive treatment for primary post-partum haemorrhage is largely dependent on the underlying cause:
Uterine Atony
- Bimanual compression to stimulate uterine contraction – insert a gloved hand into the vagina, then form a fist insider the anterior fornix to compress the anterior uterine wall and the other hand applies pressure on the abdomen at the posterior aspect of the uterus (ensure the bladder is emptied by catheterisation).
- Pharmacological measures (Table 1) – act to increase uterine myometrial contraction.
- Surgical measures – intrauterine balloon tamponade, haemostatic suture around uterus (e.g. B-lynch), bilateral uterine or internal iliac artery ligation, hysterectomy (as a last resort).
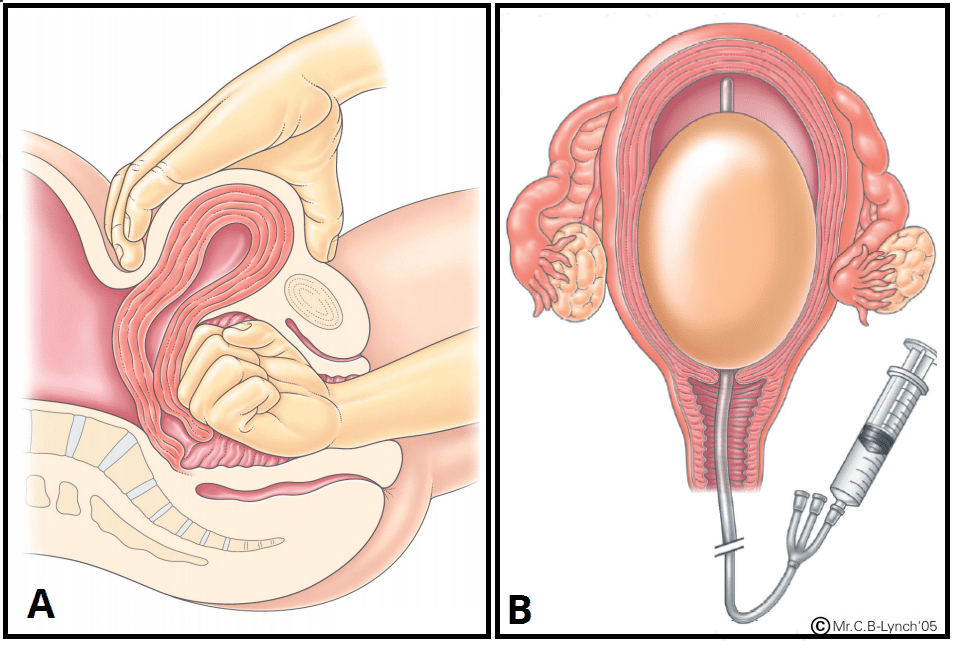
Fig 3 – Management of PPH; (a) Bimanual compression, (b) Balloon tamponade.
Trauma
Primary repair of laceration, if uterine rupture: laparotomy and repair or hysterectomy.
Tissue
Administer IV Oxytocin, manual removal of placenta with regional or general anaesthetic, and prophylactic antibiotics in theatre. Start IV Oxytocin infusion after removal.
Thrombin
Correct any coagulation abnormalities with blood products under the advice of the haematology team.
| Table 1 – Drugs used in Primary Post-Partum Haemorrhage | |||
| Drug | Mechanism of Action | Side Effects | Contraindications |
| Syntocinon | Synthetic oxytocin, act on oxytocin receptors in the myometrium | Nausea, vomiting, headache, rapid infusion à hypotension | Hypertonic uterus, severe CVS disease |
| Ergometrine | Multiple receptor sites action | Hypertension, nausea, bradycardia | Hypertension, eclampsia, vascular disease |
| Carboprost | Prostaglandin analogue | Bronchospasm, pulmonary oedema, HTN, cardiovascular collapse | Cardiac disease, pulmonary disease i.e. asthma, untreated PID |
| Misoprostol | Prostaglandin analogue | Diarrhoea | |
Prevention
Active management of the 3rd stage of labour routinely reduces PPH risk by 60%:
- Women delivering vaginally should be administered 5-10 units of IM Oxytocin prophylactically.
- Women delivering via C-section should be administered 5 units of IV Oxytocin