Read more about anatomy of the vulva here.
Background & Epidemiology:
Vulval cancer is a relatively rare condition accounting for 3–5% of female genital cancers. In the UK, it is the 20th most common female cancer and 4th most common gynaecological cancer.
Approximately 90% of vulval cancers are squamous cell carcinomas, with the main risk factor being infection with high risk human papilloma virus (HPV) and inflammation due to long standing skin conditions (such as lichen sclerosus and lichen planus). The remaining 10% are made up of primary vulval melanoma, basal cell carcinoma, Bartholin’s gland carcinoma, adenocarcinoma, and rarely, sarcoma.
Historically, vulval cancer affected only older women with the highest incidence in women more than 90 years of age. Recently, the prevalence of HPV associated vulval intraepithelial neoplasia (VIN) has significantly increased causing an increased in vulval cancer in young women. As HPV infection is a known risk factor for vulval cancer, it shares common risk factors with cervical cancer including multiple sexual partners, early age at first sexual intercourse, cigarette smoking and low socio-economic status.
Presentation:
Women with vulval cancer are usually symptomatic with the most common symptoms including: pruritis, burning, soreness, bleeding, pain or a lump.
It is uncommon to find genital warts in postmenopausal women, hence any findings should be examined to rule out cancer. Most squamous cell carcinomas are unifocal and occur on the labia majora. Other sites include the clitoris and perineum.
Diagnosis:
Diagnosis is made by biopsy. This can be performed under local anaesthetic through a Keye’s punch biopsy. It is important to take the biopsy from the edge of the lesion to include a portion of the adjacent normal epithelium.
Staging:
The natural tendency of vulval cancer is to grow by direct extension into nearby structures followed by lymphatic embolisation. Initially this is to local inguinal lymph nodes and later to femoral and the external iliac chain. Final spread to distant sites is haematogenous (through the blood stream).
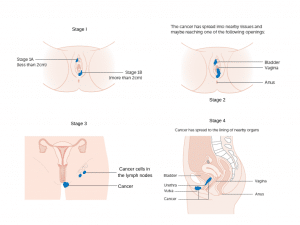
The most widely used staging system is that from the International Federation of Obstetrics and Gynaecology (FIGO):
- Stage I – Carcinoma confined to the vulva
- Stage II – Carcinoma extending to the lower third of the vagina, urethra or anus
- Stage III – Carcinoma extending to the upper two thirds of vagina or urethra, OR invasion in to bladder or rectal mucosa OR lymph nodes (non-ulcerated)
- Stage IV – ulcerated lymph nodes, disease fixed to the pelvic bone OR distant metastases
Treatment:
Vulval cancer is managed by a multidisciplinary team in a cancer centre. Surgery remains the gold standard of treatment for vulval cancer.
A patient centred approach to treatment in taken, considering the patient’s age, fitness, sexual function, tumour size, tumour site and stage of disease.
Treatment of early vulval cancer:
The main aim of surgery is complete resection of the primary tumour with adequate disease-free surgical margins and appropriate groin lymphadenectomy through separate incisions (triple incision technique).
Appropriate groin node surgery is the single most important factor in decreasing mortality from vulval cancer.
A superficial groin node dissection alone is associated with a higher risk of groin node recurrence and, therefore, the deep femoral nodes should also be removed..
Groin lymphadenectomy is associated with a high risk of complications, such as:
- Wound dehiscence
- Infection
- Lymphocyst formation
- Lymphoedema
- Immobility
- Prolonged hospitalisation
Treatment of advanced vulval cancer:
For stage III and IV disease a combination of treatment modalities are used. Surgery involves radical vulvectomy with resection of bilateral inguinofemoral lymph nodes. Most patients require post operative radiotherapy to the pelvis and groin.
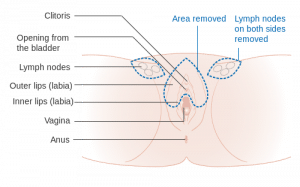
Types of vulval surgery:
- Wide local excision is recommended for small cancers.
- Partial radical vulvectomy is recommended for cancers that are confined to either side of the vulva, or the front or back only. This may mean that a large part of the vulva is removed. Usually, nearby lymph nodes are also removed.
- Complete radical vulvectomy is recommended for cancers that cover a large area of the vulva. The surgeon removes the entire vulva and the deep tissues around the vulva. Invariably the nearby lymph nodes are also removed.