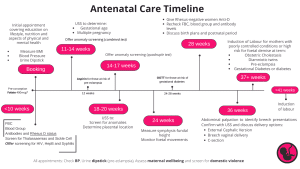
- Midwifery led care for all uncomplicated pregnancies involving 10 appointments over the course of a pregnancy for nulliparous women and 7 if it is a second pregnancy.
- Obstetrician led care If women are classed as higher risk including multiple pregnancy, maternal health problems and consists of all the midwifery appointments PLUS joint clinics to cover mental health, haematological issues, diabetes etc.
The Booking Visit is the first (and arguably the most important antenatal appointment) where an in-depth history and discussion takes place.
Vitamins in Pregnancy:
*Women at high risk of neural tube defects require a higher dose of folic acid (5mg in the first trimester, in particular those with certain medical conditions which include:
- Epilepsy
- Previous baby with neural tube defects
- Obesity with BMI over 35
- Diabetes (Type 1 and 2)
- Sickle cell disease
- Thalassemia
- Malabsorption disorders (e.g. Crohn’s disease)
- Those taking folate antagonist drugs (HIV anti-retroviral drugs, methotrexate, sulphonamides)
It should be taken ideally 3 months before pregnancy and up to the first 12 weeks.
*Offer all women Vitamin D (10 mcg) per day to reduce the risk of rickets. Women with darker skin, those from any BAME group (Black/Asian/Caribbean) or with a BMI >30 should have a higher dose.
Rhesus D status:
All women have maternal blood grouping and Rhesus typing at the booking visit. If detected:
Administer Anti-D AB to Rhesus D negative women at:
- Sensitising events (amniocentesis, antepartum bleed and abdominal trauma)
- Check the dose of Anti D required with the Kleihauer-Betke test after a sensitising event.
- Routinely offer prophylaxis at 28 and 34 weeks.
Learn more about red cell isoimmunisation here.
Foetal Growth:
Symphysis fundal height (SFH) should be measured at each antenatal appointment after 24 weeks. If there are concerns, send for an ultrasound assessment. It is important to risk assess for possible growth restriction at the first and subsequent appointments.
Other indications for these regular USS are:
- Multiple pregnancy
- BMI >35
- Large or multiple fibroids
This is because these mothers are unsuitable for SFH measurements, as abdominal palpation is unlikely to be accurate in these instances.
Consider low dose aspirin at night from 12 weeks gestation as this is known to reduce the incidence in those who are high risk of having a small for gestational age foetus.
Lifestyle Advice:
| Food | Avoid raw meat, fish, eggs, unpasteurised milk or cheeses, pate and shellfish. Fruit and vegetables should be washed to reduce toxoplasmosis |
| Exercise | Strenuous exercise is a risk factor for small for gestational age babies. Encourage exercise at the same level as pre-pregnancy if this was not vigorous, or advise to start a gentle regular programme. Advise to avoid contact or high risk sports and scuba diving. |
| Smoking | Be proactive in encouraging smoking cessation and counsel about risks. Limited evidence exists on nicotine replacement therapy but can be prescribed if the mother wishes. |
| Alcohol | High use may result in Foetal Alcohol Syndrome. To avoid this risk, the advice is to exclude completely. |
| Recreational Drugs | Most drug misuse in pregnancy has consequences to both mother and baby, however cocaine is particularly associated with adverse complications such as spontaneous abortion, placental abruption, growth restriction, and sudden infant death syndrome. Refer patients for early intervention for good outcomes. This includes: talking therapy, CBT and couples therapy. For those with addiction to opiates such as heroin and are struggling to quit, refer to the methadone programme. |
| Travel | Counsel all patients about the increased risk of venous thromboembolism (VTE) during pregnancy. Carry out individual risk assessment at booking for VTE and the need to commence prophylactic anticoagulation. Reassess at 28 weeks for those who were low – intermediate risk at booking and at each hospital admission. Advise patients even if they are low risk for VTE to be active daily and keep well hydrated to help reduce the risk of VTE. For those wishing to travel during pregnancy, recommend compression stockings and check with individual airlines on gestation limits. |
Common Problems:
Reduced Foetal Movements: Advise to immediately contact maternity services if there is any concern about baby’s movements. There should be no change to the pattern of movements or number of movements after 28 weeks gestation.
If a patient is unsure about the baby’s movements after 28 weeks, they should be advised to lie on their left side and focus on foetal movements for 2 hours. If they do not feel 10 or more movements during this time they should contact their maternity unit immediately. During the consultation assess if there is need for an ultrasound scan to assess foetal wellbeing or if delivery should be offered if the patient is term, guided by local protocols.
Nausea and Vomiting: Normally starts between the 4th and 7th week and should settle by week 20. Can suggest ginger and acupuncture, progressing to antiemetics if severe. If prolonged and severe, consider treatment for hyperemesis gravidarum
Heartburn: Alleviate by sitting up after meals, reducing fat and spice and eating smaller portions. Can suggest Gaviscon or omeprazole in severe cases.
Constipation: Encourage increased fibre and oral fluids. Can suggest bran or wheat fibre supplements.
It’s important to make sure all meetings take the opportunity to assess for mental health problems, domestic violence, sexually transmitted infections, and recreational drug use.
The MBRRACE Report
The risk of maternal death is highest among women with complex social factors according to the MBBRACE 2021 report. In general these women are classed into four categories:
- Substance misuse – alcohol and or drugs
- Teenage pregnancy
- Asylum seekers, recent migrants, refugees or those with a language barrier
- Victims of domestic abuse
The disparity of mortality and poor obstetric outcomes amongst women from some ethnic minority groups was also highlighted in the latest MBBRACE report:
- The risk of maternal death is 4 times higher in Black women, 3 times higher in women with mixed ethnic background and 2 times higher in Asian women compared with white women.
- The disparity continues once the pregnancy is over, with stillbirth rates compared with white babies more than twice as high in Black babies and 50% higher in Asian babies
- Almost twice as many stillbirths occur for women living in the most deprived areas compared with the least deprived areas.