Chlamydia is a sexually transmitted infection caused by the bacterium Chlamydia trachomatis.
It is the most common bacterial STI reported in the UK – Public Health England reported 200,288 cases in 2015 (46% of all STI diagnoses).
In this article we shall cover the pathophysiology and clinical features of a chlamydial infection, common investigations and its management.
Pathophysiology
C. trachomatis is an obligate intracellular gram negative bacterium of which there are different serotypes:
- Serotypes A-C – cause ocular infection.
- Serotypes D-K – responsible for classical genitourinary infection.
- Serotypes L1-L3 – cause lymphogranuloma venereum (LGV), an emerging infection in men who have sex with men, often resulting in proctitis.
Transmission is via unprotected vaginal, anal or oral sex. However, penetration is not always necessary – and the infection can be spread via direct skin-to-skin contact of the genitals. If infected semen/vaginal fluid enters the eye it can cause chlamydial conjunctivitis, and it is also possible for an infected mother to pass on the infection to her baby during delivery.
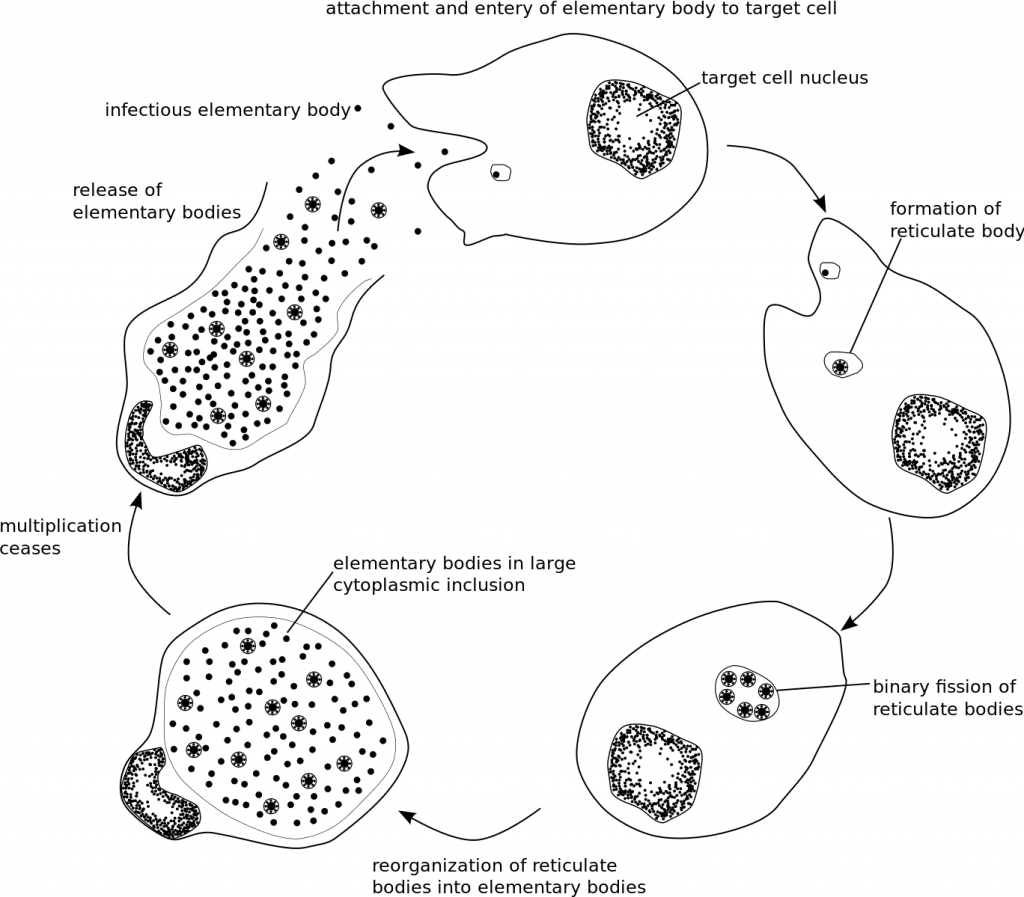
C. trachomatis enters the host cell as an elementary body (infectious form). Once inside the cell it becomes a reticular body, the non-infectious form capable of replication. Following replication, these reticular bodies mature back to elementary bodies, and following cell rupture the elementary bodies infect other cells resulting in inflammation and tissue damage.
Risk Factors
The following are risk factors associated with Chlamydia, most of which are common to other sexually transmitted infections:
- Age <25
- Sexual partner positive for chlamydia
- Recent change in sexual partner
- Co-infection with another STI
- Non-barrier contraception or lack of consistent use of barrier contraception
Clinical Features
Chlamydia is often asymptomatic, with 50% of men and 70% of women unaware that they are infected. The incubation period is typically between 7 and 21 days, after which people may become symptomatic.
In addition to the genitourinary features below, chlamydia can also infect the conjunctiva of the eye leading to irritation (chlamydial conjunctivitis), the rectum (discomfort and discharge) and the pharynx (often no symptoms).
Women

Fig 2 – Cervicitis and mucopurulent endocervical discharge in female chlamydial infection.
Symptoms
- Dysuria
- Abnormal vaginal discharge
- Intermenstrual or postcoital bleeding
- Deep dyspareunia
- Lower abdominal pain
Signs
- Cervicitis +/- contact bleeding
- Mucopurulent endocervical discharge
- Pelvic tenderness
- Cervical excitation
Men
Symptoms
- Urethritis
- Dysuria
- Urethral discharge
- Epididymo-orchitis
- Testicular pain
Signs
- Epididymal tenderness
- Mucopurulent discharge
Differential Diagnoses
A full STI screen should be undertaken for a patient presenting with chlamydia due to the common presenting symptoms of various STIs.
In particular, it is difficult to clinically differentiate between gonorrhoea and chlamydia so many NAATs now offer dual testing for both diseases. Treatment for gonorrhoea covers both N. gonorrhoeae and C. trachomatis.
Investigations
Chlamydia tests are available from sexual health clinics, GUM clinics and GP surgeries. There is also a National Chlamydia Screening Programme in England for people aged under 25 and this testing is often available from pharmacies, universities and contraception clinics.
Chlamydia is too small to be seen via microscopy so a nucleic acid amplification test (NAAT) is the recommended investigation to diagnose genital chlamydia from specimens taken at examination or by the patient:
- Women: Vulvo-vaginal swab (first choice), endocervical swab or first catch urine sample.
- Men: first catch urine sample (first choice) or urethral swab.
- If indicated, swabs may also need to be taken from the rectum, eye(s) and throat.
If positive for chlamydia, contact tracing is necessary so that the patient’s current sexual partner(s) and recent partners can be tested and treated.
Patients are recommended to have a full STI screen due to the possibility of co-infection and the similar nature of signs and symptoms.
Management
Antibiotic treatment is recommended for uncomplicated urogenital chlamydial infection:
- Doxycycline 100mg twice daily for 7 days or
- Azithromycin 1g single dose
Alternative treatment when doxycycline and azithromycin are contraindicated:
- Erythromycin 500mg twice daily for 10- 14days
- Ofloxacin 200mg bd or 400mg od for seven days
Patients are advised to avoid sexual intercourse and oral sex until they and/or their partner have completed treatment (or 7 days following azithromycin).
Test of cure is not usually required unless the patient is pregnant, compliance was poor or when symptoms persist. If aged <25, repeat testing is recommended 3 months after treatment.
Complications
In women, ascending infection can lead to salpingitis and/or endometritis which can result in pelvic inflammatory disease (PID). PID can lead to perihepatitis, ectopic pregnancy and may ultimately result in infertility.
In men, the infection can spread to cause epididymitis or epididymo-orchitis causing the testes to become painful and swollen. If left untreated, it is thought that this can affect fertility.
Chlamydia can also result in sexually acquired reactive arthritis where the joints/eyes/urethra become inflamed and this is more common in men.
Chlamydia in Pregnancy
Chlamydia may increase the risk of premature delivery with low birth weight and it is thought the infection might increase the chance of miscarriage or stillbirth. Chlamydia in pregnancy is treated with antibiotics, however doxycycline and ofloxacin are contraindicated so azithromycin and erythromycin are the drugs of choice.
If a baby contracts chlamydia they may present with inflammation and discharge in their eyes, indicative of neonatal chlamydial conjunctivitis (5-12 days after birth) and it is also possible for them to develop pneumonia (1-3 months after birth). If suspected, swabs can be taken from the eyelid or nasopharynx as indicated. Neonates are treated with oral erythromycin. Full details for the management for Chlamydia during pregnancy and for the neonate can be found in the UK national guidelines.