Antiphospholipid syndrome (APS) is an autoimmune condition in which antibodies are targeted against phospholipid-binding proteins (phospholipids are a major component of all cell membranes).
It is characterised by vascular thrombosis and/or adverse pregnancy outcomes. APS is a major treatable cause of recurrent miscarriage, with antiphospholipid antibodies present in 15% of women with recurrent miscarriage.
In this article, we shall look at the risk factors, clinical features and management of a patient with antiphospholipid syndrome.
Aetiology and Pathophysiology
Antiphospholipid syndrome is associated with the presence of antibodies targeted against phospholipid-binding proteins.
In vitro, these antibodies inhibit the assembly of phospholipid complexes – inhibiting coagulation. However, in vivo the same antibodies induce a procoagulant state.
The obstetric complications of APS are due to a number of factors:
- Inhibition of trophoblastic (precursor to the placenta) function and differentiation.
- Activation of complement pathways at the maternal–fetal interface.
- Thrombosis of the uteroplacental vasculature (late pregnancy).
Antiphospholipid syndrome can occur in isolation as a primary disease, or secondary to other autoimmune conditions; such as SLE, rheumatoid arthritis and systemic sclerosis.

Fig 1 – The vasculature of the placenta. Uteroplacental thrombosis is a consequence of antiphospholipid syndrome.
Clinical Features
Antiphospholipid syndrome is defined by thrombosis formation and/or recurrent pregnancy loss – and these are the most common clinical features.
Thrombosis may be arterial (e.g. ischaemic stroke), venous (e.g deep vein thrombosis), or microvascular – although rarely all three in the same patient. Less common thrombosis-related presentations include pulmonary embolism, myocardial infarction and retinal thrombosis.
In obstetrics, recurrent pregnancy loss (at any age) is the main feature of antiphospholipid syndrome. It is also associated with pre-eclampsia and intrauterine growth restriction (IUGR).
Other manifestations of antiphospholipid syndrome include:
- Livedo reticularis – red/blue/purple reticular pattern on skin of the trunk, arms or legs.
- Valvular heart disease – particularly aortic and mitral regurgitation.
- Renal impairment – ischaemia in the small vessels of the kidney can result in chronic kidney disease.
- Thrombocytopaenia.
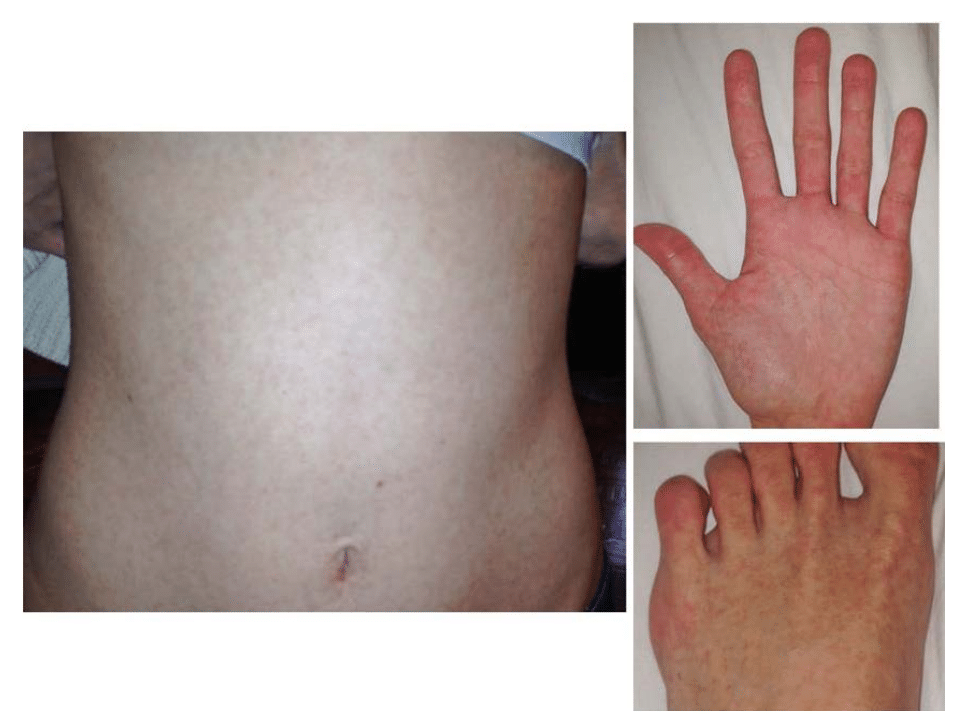
Fig 2 – Livedo reticularis: a symmetrical reticular eruption of bluish unbroken hexagons.
Catastrophic Antiphospholipid Syndrome
Catastrophic APS is a rare complication which affects approximately 1% of cases. It describes the acute formation of microthromboses, which causes infarction of multiple organs.
The exact mechanism is not known, but in 20% of cases it is triggered by major surgery, trauma or infection. Catastrophic antiphospholipid syndrome carries a mortality rate of 50%.
Differential Diagnosis
The differential diagnosis is dependent on the clinical presentation.
For a patient with arterial or venous thrombosis, other acquired and heritable thrombophilias should be considered – such as protein C or protein S deficiency.
The differential diagnoses and approach to the patient with recurrent pregnancy loss is covered here.
Investigations
The initial investigations should be used as appropriate for the presenting complaint – for example an ultrasound Doppler scan for a suspected DVT.
Testing for antiphospholipid syndrome should be considered in all women with recurrent miscarriage (≥3), atypical vascular thrombosis (e.g. unprovoked DVT), or recurrent thromboses.
There are three main blood tests used in the diagnosis of antiphospholipid syndrome:
- Anticardiolipin – detects antibodies that bind cardiolipin (a phospholipid).
- Lupus anticoagulant – measures the clotting ability of the blood. In vitro, blood containing antiphospholipid antibodies has a prolonged clotting time.
- Anti-B2-glycoprotein I – detects antibodies that binds B2-glycoprotein I (a molecule that binds with cardiolipin).
Note: Approximately 5% of healthy individuals test positive for antiphospholipid antibodies.
Diagnostic Criteria
In the UK, the diagnosis of antiphospholipid syndrome is met if one clinical criteria and one laboratory criteria is met.
Clinical Criteria:
- Vascular thrombosis – 1 or more clinical episode(s) of arterial, venous or small-vessel thrombosis.
- Pregnancy morbidity – 3 or more unexplained consecutive spontaneous abortions before 10 weeks gestation OR 1 or more premature birth(s) of a normal neonate before the 34 weeks gestation because of eclampsia or severe pre-eclampsia OR 1 or more unexplained deaths of morphologically normal fetuses at or beyond the 10th week of gestation.
Laboratory Criteria
- Lupus anticoagulant – present in the plasma on 2 or more occasions, at least 12 weeks apart.
- Anticardiolipin antibody – present in medium or high titre (>40 IgG GPL units or IgM phospholipid [MPL] units, or >99th percentile) on 2 or more occasions, at least 12 weeks apart.
- Anti-beta2-glycoprotein I – present in serum or plasma (in titre >90th percentile) on 2 or more occasions, at least 12 weeks apart.
Management
The management of antiphospholipid syndrome is centred around anticoagulation. The specific treatment is dependent on the clinical presentation of the patient, as described in Table 1.
Note: In the UK, current guidelines suggest that all women with antiphospholipid antibodies should be considered for thromboprophylaxis in the immediate postnatal period (where the risk of thrombosis is highest).
| Table 1 – Treatment of antiphospholipid syndrome | |
| Presented with recurrent pregnancy loss (≥3) | Low molecular weight heparin and low dose aspirin throughout subsequent pregnancies. |
| Presented with previous pre-eclampsia or intrauterine growth restriction | Low dose aspirin (75mg OD) throughout subsequent pregnancies. |
| Presented with vascular thrombosis
|
Long term anticoagulation with warfarin (INR 2-3). The target INR can be increased if the thrombosis was arterial.
Warfarin should be switched to low molecular weight heparin if the patient becomes pregnant or is trying to conceive. |
