Rubella (German measles) is a single stranded RNA virus, which is transmitted by airborne droplets between close contacts.
In the UK, the incidence of rubella infection has reduced dramatically since the introduction of the MMR vaccination programme. However, infection with rubella during pregnancy can have serious consequences for the fetus, and it remains an important diagnosis.
In this article, we shall look the clinical features of rubella infection, its investigations, management and complications.
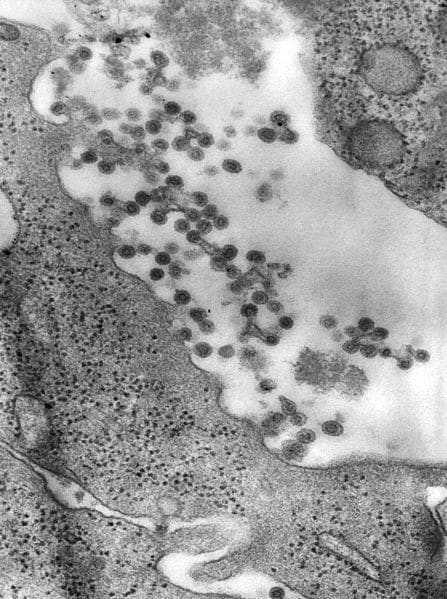
Fig 1- Negatively-stained transmission electron micrograph (TEM). Rubella virus virions can be seen budding from the host cell surface.
Antenatal Screening
Until recently in the UK, pregnant women were screened for rubella infection and immunity. Two tests were performed:
- IgM antibody – present in acute infection.
- IgG antibody – present following infection or vaccination.
In cases where neither antibody was present, the woman was encouraged to seek rubella vaccination post-delivery (rubella vaccine is a live virus, and should not be administered whilst pregnant).
From April 2016, Public Health England stopped routine screening for rubella in pregnancy – largely because of the success of the MMR vaccination programme.
Clinical Features
Maternal rubella infection is often asymptomatic.
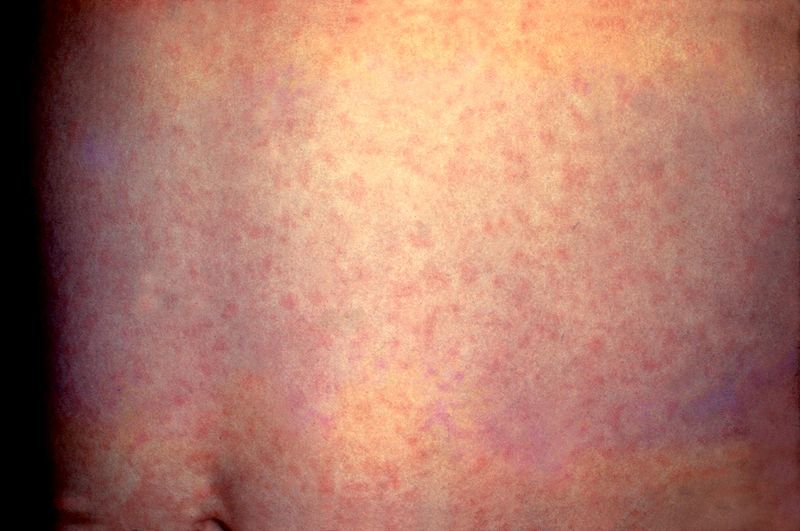
When they occur, the clinical features are non-specific, and include malaise, headache, coryza and lymphadenopathy. This can be followed by a diffuse fine maculopapular rash.
The incubation period of rubella is 14-21 days.
Investigations
In women where rubella infection is suspected, ELISA can be performed to measure rubella specific IgG and IgM:
- IgM antibody – present in acute infection.
- IgG antibody – present following infection or vaccination.
Management
Any pregnant woman with a positive rubella screen should be immediately referred to a fetal medicine specialist for counselling and further management.
Maternal
Rubella infection itself is self-limiting, and there is no treatment. Antipyretics can be given for fever.
The woman should be informed that she is infective (i.e. able to pass on the virus), from 7 days prior to the onset of symptoms to 4 days after.
Fetal
The risk of vertical transmission to the fetus, and likelihood of developing congenital rubella syndrome is determined by the gestational age at the time of infection:
| Gestation | Risk of Vertical Transmission | Risk of Congenital Rubella Syndrome |
| <12 weeks | 90% | 90%, with high likelihood of multiple defects |
| 12-16 weeks | 55% | 20%, with single defects most common |
| 16-20 weeks | 45% | 20% risk of deafness |
| >20 weeks | 45% | No additional risk |
The recommended management varies according to the gestational age at infection:
- <12 weeks – high likelihood of defects, it is reasonable to consider a termination of the pregnancy.
- 12-20 weeks – prenatal diagnosis of fetal rubella infection required. This is usually performed by RT-PCR on amniotic fluid samples.
- If transmission to the fetus is confirmed, management options include termination of pregnancy or ultrasound surveillance to identify features of congenital rubella syndrome (although some features of CRS cannot be detected by ultrasound).
- >20 weeks – No action required.
Congenital Rubella Syndrome
Congenital rubella syndrome describes the neonatal manifestation of infection with the rubella virus during pregnancy.
The clinical features can be classified into ‘present at birth’ and ‘late onset’.
Present at Birth
- Auditory Problems
- Sensorineural deafness
- Cardiac Defects
- Pulmonary Stenosis, Patent Ductus Arteriosus, Ventricular Septal Defect
- Ophthalmic Defects
- Retinopathy, Congenital Cataracts
- Central Nervous System Abnormalities
- Learning disabilities, Microencephaly
- Haematological
- Thrombocytopaenia, Blueberry Muffin Appearance
Late Onset
- Diabetes mellitus
- Thyroiditis
- Growth Hormone Abnormalities
- Behavioural Disorders

Fig 3 – Congenital cataracts, resulting from congenital rubella syndrome.